Clinical characteristics and surgical outcomes of school-age pediatric monocular retinal detachment
Beijing Tongren Eye Center; Beijing Tongren Hospital, Capital Medical University; Beijing Ophthalmology and Visual Sciences Key Laboratory, Beijing 100730, China
Abstract
?KEYWORDS: children; retinal detachments (RD); monocular
INTRODUCTION
Pediatric retinal detachments (RD) span a variety of congenital and acquired conditions which not commonly seen in adults[1-2]. The surgical and clinical management of pediatric RD is challenging because the particularities of the vitreous and the primary growth of the eye have to be considered[3-7]. Bilateral involvement has also been reported to be more common in pediatric RD, with a range of 15%-22%[8], in addition, some children may encounter monocular RD (one eye has been blind and the other comparatively healthy eye complicated with RD). School-age children is defined as children with an age of 7-14 years in China, and school-age children are at a special age for development both physically and psychologically, so monocular RD in school-age children are a special challenge to ophthalmologists demanding both surgical and psychological pressure.
Therefore, we investigated and obtained more insight into the causes, clinical and anatomic characteristics, surgical approaches, and outcomes of RD in school-age children with monocular RD
MATERIALS AND METHODS
This retrospective clinical analysis was performed at the Beijing Tongren Eye center. Ethics committee approval was obtained from Beijing Tongren Hospital ethics committee board. We reviewed charts of patients receiving surgical repair between November 2015 and May 2021. Inclusion comprised patients between 7-14 years of age with monocular RD (best corrected visual acuity of the contralateral eye was less than LogMAR 1.3). Exclusion criteria comprised primary detachment following ocular trauma and retinal re-detachments.
Gender, age, ocular history, lens status, presenting best corrected visual acuity (BCVA), previous RD on the fellow eye, symptoms and duration, RD types (tractional, rhegmatogenous, exudative), grade of proliferative vitreoretinopathy (PVR) and type of surgery (scleral buckle, pars plana vitrectomy) were collected. The surgeries were performed by only one experienced vitreoretinal surgeon.
Postoperative measures comprised functional outcomes: BCVA changes at last visit, and anatomical outcomes such as re-attachment of the central retina at the last follow-up visit.
StatisticalAnalysisStatistical analysis was performed using SPSS software (version 17.0, SPSS Inc., Chicago, IL, USA). Mann-Whitney U test and Kruskal-Wallis test were used to compare continuous variables; Fisher exact test was used to compare categorical variables between groups andPvalue of 0.05 or less was considered statistically significant.
RESULTS
This study included 27 children (27 eyes) with monocular RD, with a mean follow-up of 26.7 (6-57)mo. Overall average age at presentation was 10.63±2.30 years old and sex was predominant in boys (22/27, 82%), right eye was involved in 16 patients (16/27, 59%). Table 1 summarizes the demographic data, pathologies causing RD, and preoperative RD characteristics.
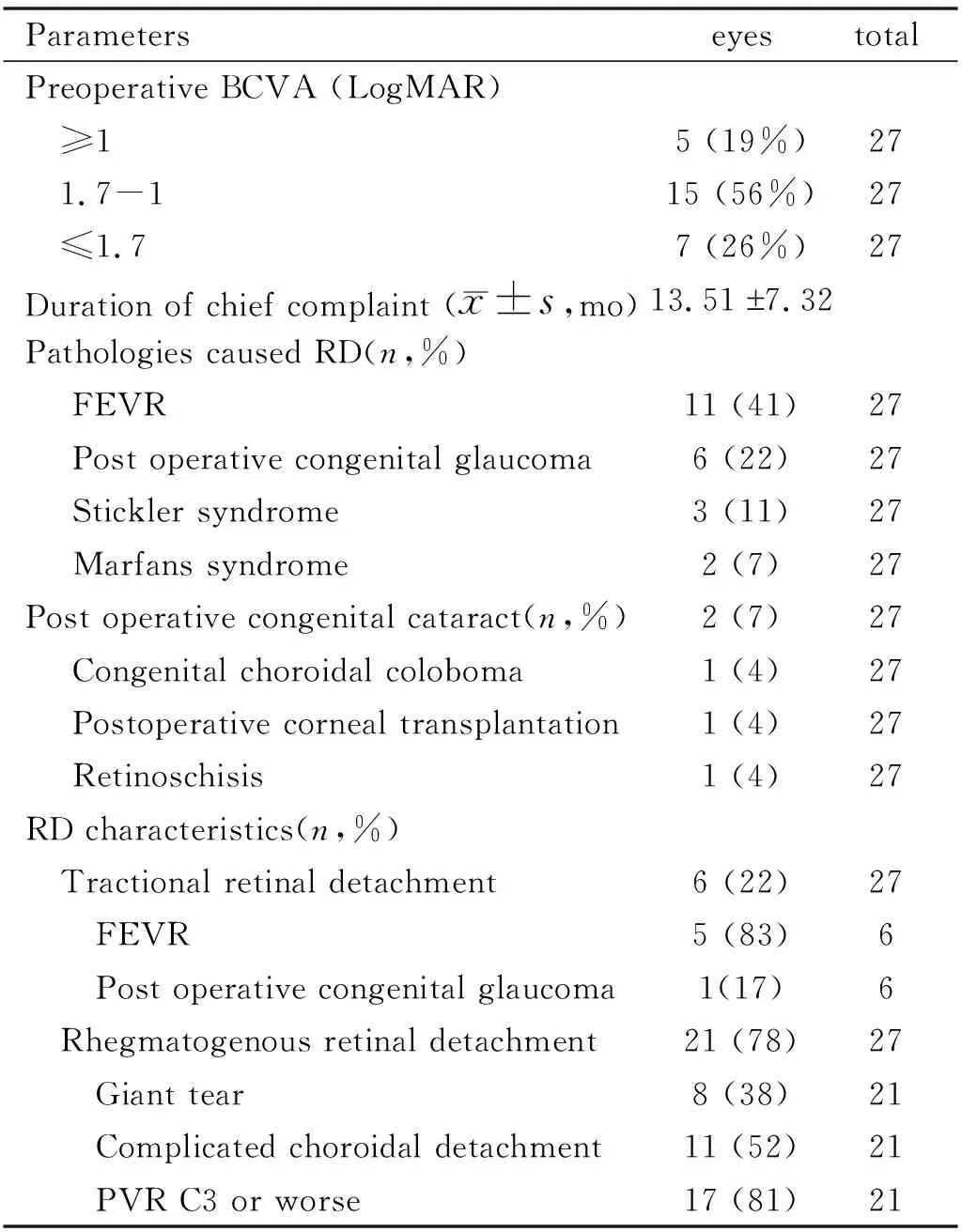
Table 1 Demographic characteristics of school-age patients with monocular RD
Most of the patients had poor preoperative BCVA: worse than LogMAR 1.7 (22/27, 82%), and three leading underlying pathologies causing RD were: familial exudative vitreoretinopathy (FEVR) (11/27, 41%) (Figure 1), postoperative congenital glaucoma (6/27, 22%) and Stickler syndrome (3/27, 11%) (Figure 2).
Postoperative retinal attachment was observed by both indirect
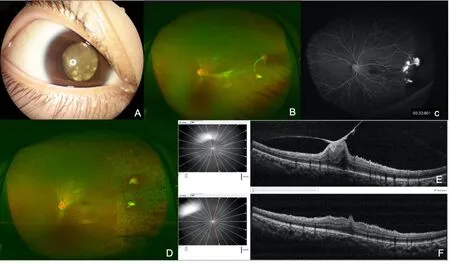
Figure 1 Ocular photographs of a 9-years-old male patient with FEVR A: Anterior segment photograph showing severe RD behind the lens of the right eye with BCVA of light perception; B: Preoperative fundus photograph showing local temporal tractional RD with neovascular membrane formation and epiretinal hemorrhage; C: Preoperative fundus fluorescence angiography showing temporal nonvascular area and local fluorescence leakage from neovascular membranes; D: Postoperative fundus photograph showing retinal attachment; E: Preoperative OCT showing macular epiretinal membrane traction; F: Postoperative OCT showing macular epiretinal membrane relievement.
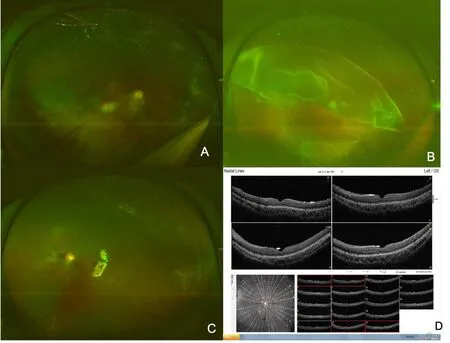
Figure 2 Ocular photographs of a 12-years-old male patient with Stickler syndrome A: Fundus photograph showing postoperative attached retina of the right eye with BCVA 0.02; B: Preoperative fundus photograph RD with superior giant tear of the left eye with BCVA: hand move (HM); C: Postoperative fundus photograph showing retinal attachment with silicon oil tamponade of the left eye with BCVA of 0.2; D: Postoperative OCT showing retinal attachment with normal macular fovea one month later.
Rhegmatogenous retinal detachment (RRD) comprised 78% (21/27) of the patients, of which 38% (8/21) complicated with giant retinal tear, 52% (11/21) complicated with simultaneous choroidal detachment, and 81% (17/21) of the patients had PVR C3 or worse.
The main type of surgery was pars plana vitrectomy (PPV) (23/27,85%), and of which 83% (19/23) of the patients received silicone oil tamponade, and 74% (17/23) of the patients combined with lensectomy. Seven patients underwent vitrectomy combined with simultaneous endocyclophotocoagulation, of which 6 patients with RD complicated with congenital glaucoma and 1 patient with RD complicated with corneal transplantation, all these 7 patients had high intraocular pression (IOP) before RD happened and needed at least 2 kinds of anti-glaucoma eye drops (Table 2) (Figure 3).
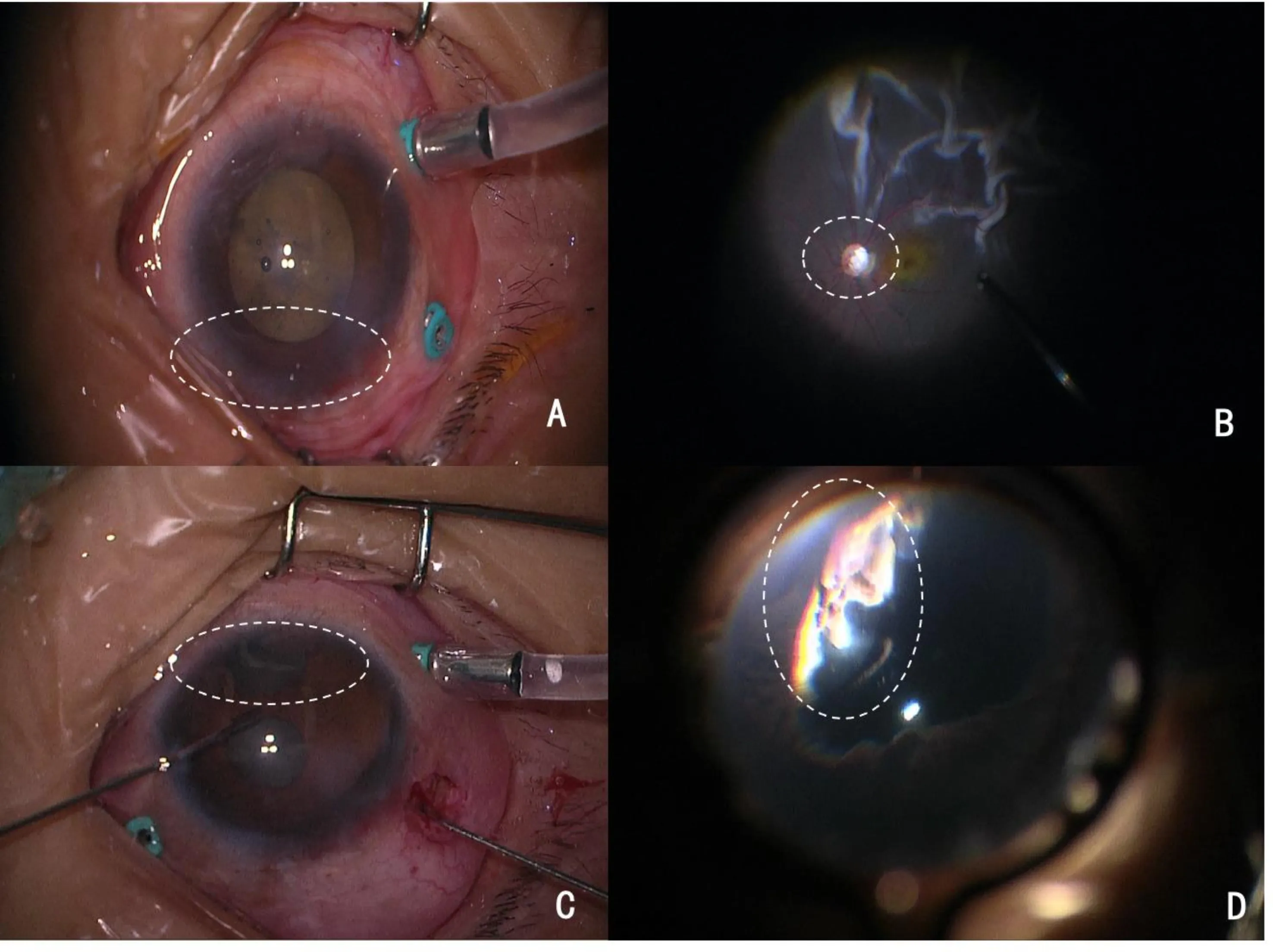
Figure 3 Ocular photographs of 8-years-old male patient with postoperative congenital glaucoma complicated with RD of the right eye, with left eye BCVA: light perception A: Intraoperative anterior segment photograph showing expanded corneal limbus (white dotted circle); B: Intraoperative fundus photograph showing pale optic disc caused by long-term high intraocular pressure (white dotted circle); C: Intraoperative anterior segment photograph showing peripheral iridectomy (white dotted circle); D: Intraoperative photograph showing endocyclophotocoagulation (white dotted circle).
C3F8 (14%) was used for gas tamponade in 4 children who can cooperate with face-down position, and also had RD with holes or breaks in the superior retina.
There were 21 of the 27 patients (21/27, 78%) had postoperative BCVA worse than LogMAR 1.7 at final visit, and although most of the patients had reattached retina at last visit, 41% (11/27) of the patients still remained status of silicone oil tamponade, those patients with final silicone oil removal had an average interval of 6.47mo between silicone oil injection and silicone oil removal (Table 2).
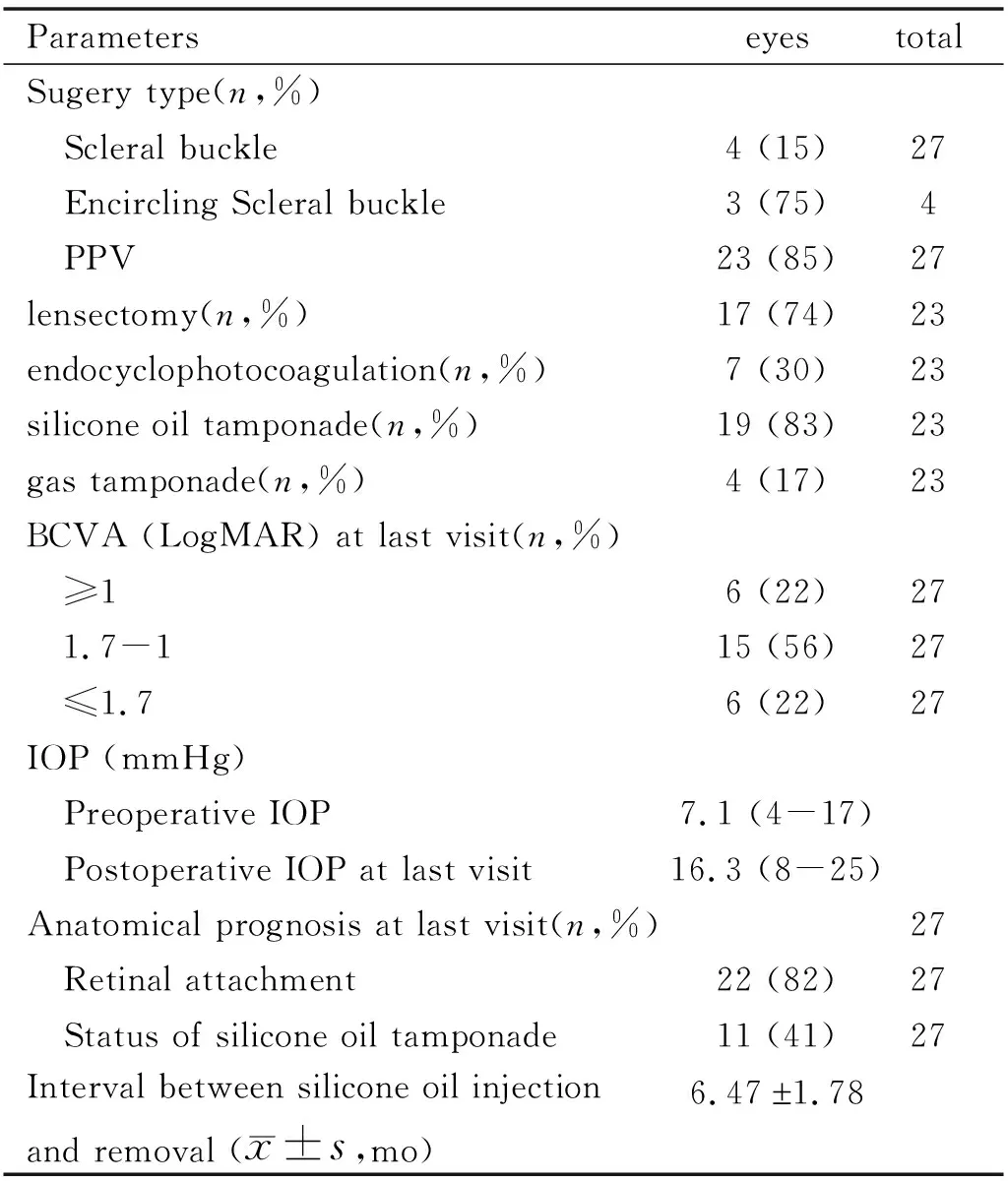
Table 2 Treatment procedures and prognosis of school-age patients with monocular RD
Average postoperative IOP was high than that of preoperative IOP (Table 2), 13 eyes (13/27, 48%) had high postoperative IOP and their average IOP at 1wk after operation was 32.1 mmHg, anti-glaucoma medicines were used and 3 patients still underwent further cyclophotocoagulation. IOP were all controlled at last visit with 2 patients still needed one kind of anti-glaucoma eye drops.
ophthalmoscope and OCT, color Doppler image was used to reassure retinal attachment for patients with opaque media. Seven eyes (7/27, 26%) had postoperative RD, further vitrectomy combined with silicon oil tamponade was given but 5 eyes (5/27,19%) still had RD at last visit.
Phakic eye was found in 18 preoperative patients, of which 5 patients (5/18, 28%) complicated with postoperative cataract and underwent further phacoemulsification. No other postoperative complications such as vitreous hemorrhage or endophthalmitis was found.
DISCUSSION
Most studies evaluated pediatric RD below 18 years to define and investigate different predisposing factors, clinical characteristics, and prognosis[9-11]. However, it is much more important to distinguish RD in school-age children, as congenital eye diseases can still play a role in those patients, especially those with monocular RD, and a comparatively successful surgical management of those patients was extraordinarily essential and meaningful. To our knowledge, no other study has investigated school-age patients with monocular RD. We specifically chose this age group to analyze whether and to what extent the various causes of RD play a role.
Pediatric monocular RD was mostly related to hereditary or congenital ocular abnormalities in our study. Previous study revealed that pediatric RD always complicated with congenital developmental anomalies, and the reported incidence ranges from 12% to 56%[12]; Soheilianetal[13]also reported in a retrospective case series of 127 eyes that in children below the age of 10 years congenital developmental anomalies comprise 52.5% of RD. The pathological basis causing RD of these patients were reported to be related to peripheral retinal degeneration (lattices with or without atrophic holes, retinal tears or retinal breaks) and /or vitreoretinal tractions that related to bilateral congenital or developmental anomalies[14-15]. In our study, persistence and deterioration of the pathological basis may induce blindness of one eye at an early period and may eventually induce RD of the other eye, so pediatric patients with monocular RD should remind ophthalmologists to explore the underlying hereditary or congenital etiologies such as FEVR, Stickler syndromeetal.
Pediatric patients with monocular RD presented with more cases with RRD with severe PVR reaction and simultaneous choroidal detachment in our study. Usually all forms of RD (rhegmatogenous, tractional, and exudative) could be found in the pediatric patients, more RRD were found in the age group older than 6 years[16]; previous studies also reported that a complete and foveal-off RD with much more severe PVR reaction already existed at the initial presentation of pediatric RD compared to RD in adult patients[17]. The high percentages of severe PVR reaction in our study may be related to the high rate of underlying congenital or developmental eye diseases such as FEVR, Stickler syndrome or Marfan syndrome etc, which could cause extensive abnormal peripheral retinal degenerations. Complicated simultaneous choroidal detachment in our patients may be related to the inherent abnormal blood-retinal barrier induced by developmental eye diseases or previous intraocular surgeries such as congenital glaucoma.
PPV combined with silicon oil tamponade was mostly indicated in pediatric patients with monocular RD. Although scleral buckle is preferred for pediatric patients with mild RD because of its associated advantages such as less trauma and preservation of ocular integrity[18-22], PPV is a prerequisite surgical choice for pediatric patients characterized with severe PVR reaction, giant tear and simultaneous choroidal detachment[23]. During PPV, posterior vitreous detachment (PVD) can be performed and posterior hyaloid can be completely removed to minimize possibilities of postoperative contraction of the residual vitreous, postoperative PVR reaction, and severe epiretinal membrane formation; all the retinal breaks can also be found and treated at the same time using intraocular illumination.
Poor postoperative visual outcomes despite comparatively high rate of anatomical retinal reattachment were common for pediatric patients with monocular RD in our study, this poor VA prognosis was similar to the previous studies for pediatric RD[24-26]. There were 21 patients of the 27 patients (21/27, 78%) had postoperative BCVA worse than LogMAR 1.7 at final visit in this study, possible explanations for the poor VA for many of those patients in our study include congenital structural abnormality, severe coexistent eye diseases, macula involvement, poor initial preoperative vision acuity and amblyopia. However, this comparative poor VA results were still very important and meaningful for monocular pediatric patients in their daily life.
Pediatric patients with monocular RD had lower rate of postoperative retinal attachment of 81.5% compared to that of adult patients, previous studies have reported similar results with final anatomical success rate of 72%-87% for pediatric RD patients[27]. Pediatric patients might be expected to have worse anatomical prognosis as they often present with more chronic RD by not recognizing or being able to communicate their loss of vision[28-34]. In addition, they often had associated specific clinical characteristics such as more extensive RD with severe PVR, macular involvement and coexistence of ocular abnormalities, which may portend worse outcomes.
High postoperative IOP, retinal redetachment and complicated cataract were main postoperative complications for pediatric monocular RD patients. Postoperative high IOP was common for RD patients[35], especially for patients with high percentage of simultaneous congenital glaucoma in our study. We also chose simultaneous endocyclophtocoagulation during PPV to control postoperative IOP using a standard endolaser probe for patients with high IOP before RD happened, during the endocyclophtocoagulation we could visualize the treatment target and directly deliver laser power specifically to the epithelium of biliary body. Reasons for high rate of postoperative cataract may be high percentages of congenital ocular abnormalities and high rate of silicon oil tamponade. Patients with severe complicated cataract underwent further surgery either during silicon oil removal or by another independent cataract surgery.
This retrospective study has many limitations including its relatively short time of follow-up, retrospective nature and the potential bias that patients in our study were mostly referred from other hospitals and had very severe pathologies. High percentage of silicone oil tamponade was still found at last visit, so the anatomical success rate of 82% may be lower given longer time of follow-up. With the long-life span of these patients, further studies with longer-term follow up and more paralleled cases are necessary to delineate the long-term visual and anatomical prognosis of monocular RD in children. But our study has its advantages of being the largest series of studies investigating the clinical characteristics of patients with school-age pediatric monocular RD.
In summary, school-age pediatric monocular RRD is often associated with underlying congenital or hereditary conditions. And those children often presented with extensive RD with severe PVR reaction and always needed vitrectomy combined with silicon oil tamponade, and also with poor visual and anatomical short-term prognosis. Our results should assist the ophthalmologist in predicting treatment difficulties and poorer prognosis for patients with school-age pediatric monocular RD and managing the expectations of anxious parents and pediatric patients to ensure continued follow-up to enhance final surgical outcomes.
- 國際眼科雜志的其它文章
- Predictive index based on minimum corneal thickness and symmetry index back of Sirius for early diagnosis of keratoconus
- 結(jié)膜松弛癥球結(jié)膜成纖維細(xì)胞的原代培養(yǎng)及形態(tài)學(xué)觀察
- 基于EDI-OCT技術(shù)觀察遠(yuǎn)視性弱視兒童脈絡(luò)膜結(jié)構(gòu)的變化
- 飛秒激光輔助下白內(nèi)障手術(shù)對(duì)角膜內(nèi)皮細(xì)胞影響的Meta分析
- OCTA評(píng)價(jià)無糖尿病視網(wǎng)膜病變患者黃斑區(qū)微循環(huán)特征的Meta分析
- 基于加權(quán)基因共表達(dá)網(wǎng)絡(luò)分析非動(dòng)脈炎性前部缺血性視神經(jīng)病變的關(guān)鍵基因

