Feedback of inter-hospital transfer of patients under high-f low nasal cannula oxygen therapy
Emilien Arnaud, Sylvain Leclere, Martin Petitprez, Gilles Vincent, Christine Ammirati
Department of Emergency Medicine, Amiens-Picardy University Hospital, Amiens 80000, France
Severe forms of coronavirus disease 2019 (COVID-19)can lead to hypoxemic pneumonia and the need for treatment with high-flow nasal cannula (HFNC) oxygen therapy.This treatment decreases the need for subsequent invasive ventilation in patients with hypoxemic pneumonia. The oxygen flow in the nasal cannula is driven pneumatically or using a turbine. Oxygen and air are mixed (giving the fraction of inspired oxygen [FiO]) and propelled at up to 80 L·min. The propelled gases must be heated and humidif ied.HFNC system is not intended for use outside a hospital environment.
The COVID-19 has been spreading quickly, and almost all countries and regions around the world have been aff ected.In France, the COVID-19 pandemic led to the saturation of intensive care units, a lack of beds,and thus the need for patient transfers. Patients on HFNC with no indication for immediate invasive ventilation cannot be transferred using conventional oxygen therapy.However, the use of invasive ventilation for interhospital transfers raises ethical questions. With a view to avoiding transfers with intubation,the Somme County Emergency Medical Service (SAMU80, part of Amiens-Picardy University Hospital [CHU-AP], Amiens, France)studied the feasibility of transferring patients on HFNC.
METHODS
Firstly, an intensive care physician and an emergency physician made a clinical assessment of each candidate for transfer and determined whether invasive ventilation was essential or not. The ROX score (the oxygen saturation to inspired oxygen fraction ratio, divided by the respiratory rate) was used to assess transferability on HFNC.
The SAMU80 estimated the transfer duration from the mean duration of previous patient transfers over similar routes. The calculation of the quantity of oxygen required was based on the maximum flow rate with 100% FiO, multiplied by the estimated travel duration and with an extra 20% safety margin. The ambulance loaded two 3 mtanks and four 1 mtanks. During the first ward-ambulance transfer, the SAMU80 used the in-hospital oxygen tanks. HFNC was delivered via a battery-powered turbine-propelled system (Monnal T60? [MT60], Air Liquide Medical Systems, France)or a pneumatic system (a digital manometer plugged directly into the oxygen tank upstream of the heater).In both cases, an MR850 heater (Fisher & Paykel Healthcare, New Zealand) was placed upstream of a disposable patient circuit. The heater was unplugged during the transfers to and from the ambulance. The MT60’s batteries were fully charged, and the ventilator ran on battery power throughout the transfer. Two moisture exchangers were placed between the disposable patient circuit and the respirator. The patient wore an FFP1 mask over the nasal cannula, and all the members of the SAMU80 team wore personal protection equipment (an FFP2 mask, hairnet, eye shield, and disposable coveralls).
The HFNC transfer was considered to have been successful if the patient did not require intubation and did not die in the two days following the transfer. I n line with the French legislation on retrospective studies of clinical practice, the study protocol was approved by a local committee with competency for research not requiring approval by an institutional review board(Amiens, France; reference: PI2021_843_0173).
RESULTS
The first patient (Table 1) was a 57-year-old man with multiple comorbidities (chronic pancreatitis,and quadriparesis following spinal trauma). Thirteen days after the onset of COVID-19 symptoms, he was transferred from CHU-AP to a nearby private-sector clinic (4 km away), using a pneumatic air-propelled HFNC. The ROX score was 4.54 and the attending physicians chose to initiate the HFNC transfer. No complications occurred during the transfer, and approximately 1,000 L of oxygen was used. There was no indication for intubation but the patient died 11 days after the transfer.
The second patient was a 37-year-old man with B cell lymphoma in remission. Eight days after the onset of COVID-19 symptoms, he was transferred from Saint-Quentin General Hospital to CHU-AP (76 km away)using a turbine-propelled HFNC system. Even though the ROX score was 2.71, the attending physicians decided to transfer the patient on HFNC, with the patient’s consent.No complications occurred during the transfer, and approximately 3,200 L of oxygen was used. The patient did not require intubation and was alive 7 days after the transfer.
The third patient was a 68-year-old woman with chronic obstructive pulmonary disease. Ten days after the onset of COVID-19 symptoms, she was transferred from CHU-AP to Lille University Medical Center (114 km away) using turbine-propelled HFNC. The ROX score was 3.68, and the physicians decided to transfer the patient using HFNC.No complications occurred during the transfer. The transfer consumed approximately 5,200 L of oxygen.
The first problem encountered was how to monitor the amount of oxygen remaining. With a flow rate of 80 L·min, the digital manometers are not calibrated to calculate the remaining amount. The MT60 monitors the FiOdelivered to the patient and sounds an alert when the oxygen tank is empty. The pneumatic airpropelled HFNC system also sounds an alert when the tank is empty. The second problem was related to changing the oxygen tank, which led to a short period of desaturation for two patients, although there were no clinical complications. The third problem was the absence of a heater during the ambulance-ward transfer.The heater does not have a battery and requires mains electricity. With maximum flow, the heater falls from a temperature of 37° to room temperature within a few minutes of disconnection. To counter this problem,the setpoint temperature was set to the highest value before disconnection, the ambulance-ward transfer was as short as possible, the heater was covered with a survival blanket, and the heater was the first equipment to be plugged in on arrival. No immediate clinical complications were observed during these ambulanceward transfers.
DISCUSSION
The transfer of patients on HFNC was feasible, and no immediate clinically observable complications arose.The SAMU80 had to plan the transfer carefully: the status of the transferred patient, the oxygen requirement for the journey, the shortest ambulance-ward transfer route, etc. The patient’s transferability must be evaluated by an experienced physician. Based on the results of our pilot study, we have drafted a checklist (Figure 1) for HFNC transfers.
With regard to safety, there is no consensus on risk of droplet dispersion by patients with COVID-19.Li et alcompared droplet dispersion with a simple mask and HFNC at similar distances (11 cm and 17 cm,respectively) and concluded that the use of HFNC did not increase the risk of microbiological contamination.Leonard et alsuggested that the risk of dispersion could be reduced by placing an FFP1 mask on the patient. Morin et aland Carteaux et alsuggested using the Boussignac continuous positive air pressure system (equipped with a moisture exchanger to prevent dispersion) and demonstrated that the device was safe.
These complex transfers can avoid the need to(1) initiate invasive ventilation that is not otherwise indicated; and (2) provide the patient with an intensive care bed. The absence of invasive ventilation avoids the complications of mechanical ventilation.
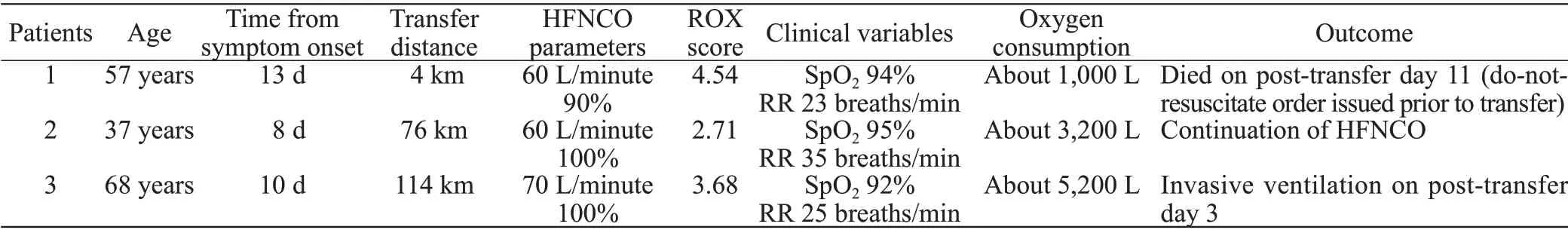
Table 1. The patients’ characteristics
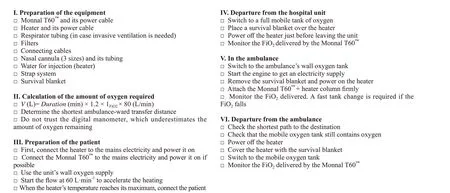
Figure 1. Checklist for transferring a patient receiving high-f low nasal cannula oxygen therapy.
CONCLUSIONS
Our pilot study shows that transferring patients on HFNC is possible but we only evaluate the shortterm impact. A longer-term, prospective study of the transfer of a larger number of patients on HFNC is now warranted.
None.
The study protocol was approved by a local committee with competency for research not requiring approval by an institutional review board (Amiens, France; reference:PI2021_843_0173).
The authors declare that they have no competing interests.
EA proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
 World Journal of Emergency Medicine2022年3期
World Journal of Emergency Medicine2022年3期
- World Journal of Emergency Medicine的其它文章
- Mortality-related electrocardiogram indices in methanol toxicity
- The combination of creatine kinase-myocardial band isoenzyme and point-of-care cardiac troponin/contemporary cardiac troponin for the early diagnosis of acute myocardial infarction
- Increasing angiotensin-converting enzyme (ACE) 2/ACE axes ratio alleviates early pulmonary vascular remodeling in a porcine model of acute pulmonary embolism with cardiac arrest
- Shrinking lung syndrome in autoimmune inflammatory diseases: A case series and review of literature
- Traumatic tension pneumocephalus: A case report
- Blunt myocardial injury and gastrointestinal hemorrhage following Heimlich maneuver: A case report and literature review
