Complications of modern pancreaticoduodenectomy: A systematic review and meta-analysis
Stmtios Kokkinkis , Evngelos I Kritsotkis , Neofytos Mliotis , Ionnis Krgeorgiou ,Emmnuel Chrysos , Konstntinos Lsithiotkis ,?
a Department of General Surgery, University General Hospital of Heraklion, Heraklion, Crete 71110, Greece
b Laboratory of Biostatistics, Division of Social Medicine, School of Medicine, University of Crete, Heraklion, Crete 71110, Greece
Keywords:Pancreaticoduodenectomy Postoperative complications Meta-analysis Postoperative pancreatic fistula
A B S T R A C T
Introduction
Pancreaticoduodenectomy (PD) is considered one of the most complex procedures in general surgery and it is associated with considerable morbidity. In the last decades, PDs have been mostly performed in high-volume centers and this centralization has led to important reduction in postoperative mortality [1–3] . Moreover,the perioperative management of PD patients has undergone significant advances, such as the widespread availability of interventional radiology that leads to less invasive management of major complications and fewer reoperations [ 4 , 5 ] and the use of prehabilitation programs that show promising results regarding postoperative outcomes [6] . Enhanced recovery after surgery (ERAS) pathways have also established their usefulness in PD patients, with reported reduction in overall morbidity and the length of stay [7] .Moreover, internationally accepted criteria are now widely used to better define complications following PD [ 8 , 9 ], allowing for precise recording and grading.
Due to these new parameters, the management and the outcomes are substantially different compared to those in the previous decades. This systematic review aimed to assess the preand intraoperative data, and postoperative complications of modern PDs in pancreatic centers worldwide in the last decade, to provide useful benchmarks for centers dealing with lower PD volumes and facilitate patient counseling preoperatively.
Methods
This study is compliant with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement [10] . A search in PubMed from January 2010 to April 2020 was performed.The bibliographies of relevant systematic reviews and original reports were screened in search of additional studies.
Including criteria for studies
Typesofstudies
Both randomized control trials and non-randomized clinical studies were included. Non-randomized studies, either comparative or non-comparative, were considered eligible for this review if the complications were recorded prospectively based on predetermined criteria. Studies based on registry data were also eligible.For inclusion, a minimum of 100 PDs, a follow-up for complications of at least 30 days and a study period between January 2010 and April 2020 were required. Only studies written in English were considered. We excluded case reports, case series, systematic reviews, meta-analyses, non-clinical studies and publications in nonpeer reviewed journals.
Typesofparticipants
Adult patients undergoing PD either for suspected or confirmed neoplastic lesions were included. Patients undergoing PD for trauma or a known non-neoplastic disease (such as chronic pancreatitis) were excluded. PDs performed on animals were excluded.
Typesofinterventions
Open and minimally-invasive PDs were included, regardless of the reconstruction method used. Classic Whipple procedures and pylorus-preserving PDs were included. Only PDs with curative intent were included, when no additional operations were performed, except for vascular resections. Studies in which the details of the operative technique were unclear or not reported were excluded.
Typesofoutcomemeasures
Outcomes of interest were postoperative complications, both surgical and medical, postoperative mortality and length of hospital stay after PD.
Data collection and analysis
Three authors (Kokkinakis S, Karageorgiou I and Maliotis N) independently assessed all identified articles based on our eligibility criteria. Any discrepancies involving relevant articles were discussed between authors until agreement was reached. If no agreement was reached between authors, Lasithiotakis K served as arbitrator. Articles were included if all patients or at least a subgroup of patients involved in the study fulfilled our eligibility criteria. According to the PRISMA criteria, identified articles were first screened based on their titles. The remaining articles were screened based on their abstract, which had to be compliant to our eligibility criteria. Thirdly, full-texts of all articles that successfully passed the second level of screening were reviewed in detail,to identify the studies to be included in the final analysis.
Data extraction and management
Data were extracted using a predetermined standardized form by 3 authors (Kokkinakis S, Karageorgiou I and Maliotis N) independently. Any disagreements regarding the extracted items were discussed between authors until a consensus was reached, while Lasithiotakis K served as arbitrator. If relevant data were missing or unclear for extraction, the study authors were contacted for clarification. Data extracted included the following information.
(1) Publication data: author, year of publication, country of origin, study period, number of patients, study design, aim of the study.
(2) Pre- and intraoperative data: summary statistics for age, body mass index (BMI), American Society of Anesthesiologists (ASA)score, preoperative biliary drainage, operative time, blood loss,intraoperative transfusion, concomitant vascular resection, percentage of patients with soft pancreas and small pancreatic duct (diameter < 3 mm).(3) Surgical complications: mortality (in-hospital, 30- and 90-day),rate of overall complications, serious complications, postoperative pancreatic fistula (POPF, overall and clinically-relevant), delayed gastric emptying (DGE), biliary leak, post-pancreatectomy hemorrhage (PPH), intra-abdominal abscess formation, surgical site infection (SSI), postoperative pancreatitis, reoperation, readmission (30-day and 60/90-day) and length of postoperative hospital stay.
(4) Medical complications: cardiac, respiratory, neurologic complications, venous thromboembolism (VTE), urinary tract infection(UTI), acute renal failure (ARF) and sepsis.
(5) The definitions used for each complication were also recorded.
Assessment of risk of bias in included studies
Risk of bias in randomized trials was assessed using the revised Cochrane tool RoB2 [11] . The methodological index for nonrandomized studies (MINORS) was used in order to evaluate the quality of observational studies [12] , with a maximum score of 16 for non-comparative and 24 for comparative studies. The signaling questions were asked independently by 2 authors (Kokkinakis S and Maliotis N), and any discrepancies were resolved by a third author (Lasithiotakis K).
Meta-analysis methods
Pooled estimates of single group proportions and means were obtained as weighted averages using the random-effects inversevariance model with DerSimonian and Laird estimate of the between-study variance. The Freeman-Tukey double arcsine transformation was utilized to stabilize the variances when pooling proportions [13] . Sample means and standard deviations were estimated from commonly reported quantiles in individual studies when required [14] . Higgin’sI2index was used to quantify the heterogeneity in reported proportions and means between the studies. The statistical significance of heterogeneity was tested using Cochran’s Q statistic. Subgroup analysis and univariate randomeffects meta-regression were used to examine if variation in reported complication rates may be explained by differences in study characteristics (country of origin, study design, data collection method, type and pathology of PD, and risk of bias rating) or characteristics of the patients (average age, operative time and blood loss, and proportions of ASA categories, biliary drainage, transfusion, soft pancreas, small pancreatic duct and vascular resection).Multivariate meta-regression was pursued to assess independent contributions from characteristics that were found to be statistically significant (P< 0.05) in univariate analysis, provided that at least 10 additional studies were available for every degree of freedom modelled [15] . All analyses were carried out in STATA (Version 17; Statcorp, College Station, TX, USA).
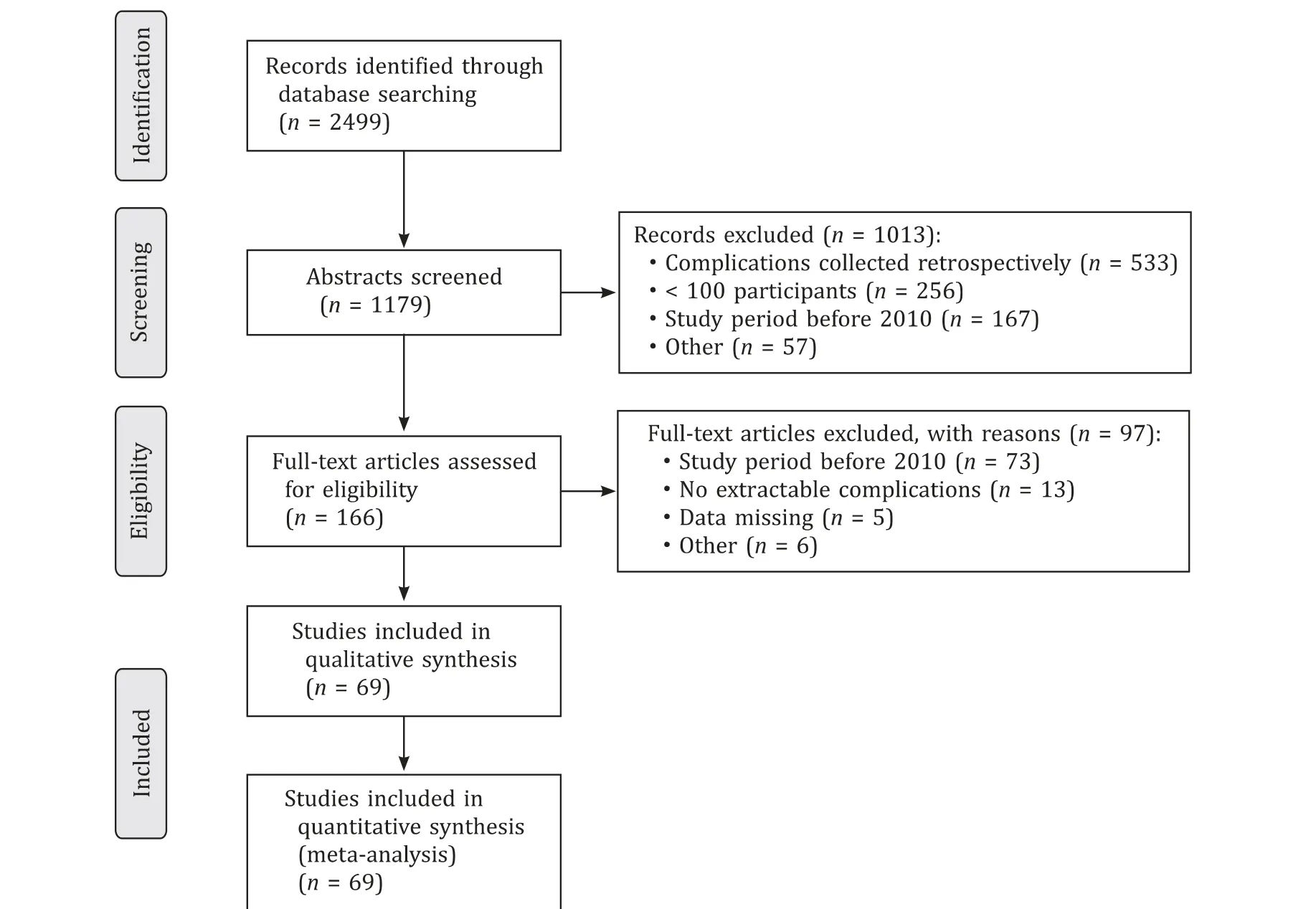
Fig. 1. PRISMA flowchart depicting the inclusion process for the systematic review.
Results
Description of studies
The literature search yielded 2499 studies. Following title and abstract screenings, 166 studies were eligible for full-text screening. Of those, 97 were excluded according to the criteria and 69 studies were deemed eligible for data extraction and analysis. The flowchart depicting our inclusion process is shown in Fig. 1 . Of the included studies, 20 were randomized controlled trials [16–35] and 49 were non-randomized [36–84] . Six studies were based on registry data [ 4 8 , 51 , 57 , 6 8 , 71 , 77 ].
Risk of bias
After the assessment of the risk of bias in the included studies, 6 randomized trials (30%) were deemed as low-risk studies,9 (45%) raised some concerns, and 5 (25%) were deemed to have high-risk bias based on the RoB2 tool. The mean MINORS for nonrandomized studies were 19.0 ± 1.2 for comparative studies and 12.0 ± 0.9 for non-comparative studies, indicating high-risk of bias in both cases.
Meta-analysis
Sixty-nine studies with 63 229 participants were analyzed. Preand intraoperative characteristics of the included patients are reported in Table 1 . The pooled mean for patient age was 63.7 years (95% CI: 62.3–65.2;I2= 98.8%), mean operative time was 366.9 min (95% CI: 348.3–385.6;I2= 99.4%) and mean blood loss was 424.6 mL (95% CI: 379.1–470.0;I2= 98.9%).
Postoperative surgical and medical complications are shown in Table 2 . The pooled rate of all complications combined was 54.7%(95% CI: 46.4%–62.8%;I2= 99.4%), while the rate of serious complications was 25.5% (95% CI: 21.8%–29.4%;I2= 92.9%). The pooled risk of 30-day mortality from 22 studies was 1.7% (95% CI: 0.9%-2.9%;I2= 95.4%) ( Fig. 2 ). The risk of CR-POPF was 14.3% (95%CI: 12.4%–16.3%;I2= 92.0%; 57 studies) ( Fig. 3 ). The pooled mean length of hospital stay after PD was 14.8 days (95% CI: 13.6-16.1;I2= 99.3%; 48 studies) ( Fig. 4 ). The classification proposed by Clavien-Dindo [85] was most frequently used to define overall complications, with serious complications usually being defined as Clavien-Dindo grade > II, while International Study Group on Pancreatic Surgery (ISGPS) criteria [ 8 , 86 , 87 ] were mostly used to define POPF, DGE and PPH.
Subgroup analyses did not detect significant variation in complication rates according to the different definitions for complications reported in the studies. Univariate random-effects metaregression showed that heterogeneity was partially explained by differences in characteristics of the studies and their patients,such as continent of origin of the study, study design (multicenter or single center), patient age and ASA score ( Table 3 ). The 30-day mortality was significantly higher in studies performed in North America [mean difference (MD) = 3.4%, 95% CI: 1.0%-5.9%;P= 0.005] and lower in Asian studies (MD = -3.5%, 95% CI: -5.8%to -1.2%;P= 0.003). 30-day mortality was also higher in studies that included minimally invasive PDs (MD = 3.7%, 95% CI: 1.2%-6.2%;P= 0.004) and those involving only malignant pathologies(MD = 3.6%, 95% CI 1.1%-6.0%;P= 0.005). Mean length of stay was significantly higher in European studies (MD = 2.7 days, 95% CI:0.6-4.8;P= 0.010), Asian studies (MD = 3.3 days, 95% CI: 0.5–6.0;P= 0.022), multicenter studies (MD = 4.8 days, 95% CI: 2.4–7.3;P< 0.001) and registry-based studies (MD = 8.4 days, 95% CI:1.6–15.1;P= 0.015), while it was lower in North American studies(MD = -6.7 days, 95% CI: -8.9 to -4.5;P< 0.001). A 10% increase in ASA III/IV proportion was associated with a higher incidence ofoverall complications (MD = 3.4%, 95% CI: 1.4%–5.3%;P= 0.001).The number of retrieved studies was not enough to justify multivariate meta-regression for complications other than CR-POPF. Results of meta-regression analyses for other complications are presented in Tables S1–7. CR-POPF incidence was significantly higher in European studies (MD = 5.8%, 95% CI 1.7%–9.9%;P= 0.005)and multicenter studies (MD = 5.6%, 95% CI 1.8%–9.4%;P= 0.004),while a 5-year increase in average patient age was associated with a 5% increase in CR-POPF (95% CI: 3.0%-7.0%;P< 0.001). However,in the multivariate analysis (Table S8) only the average patient age retained a significant and independent association with CR-POPF incidence (adjusted MD = 4.3% per unit increase, 95% CI: 1.5%–7.1%;P= 0.002).
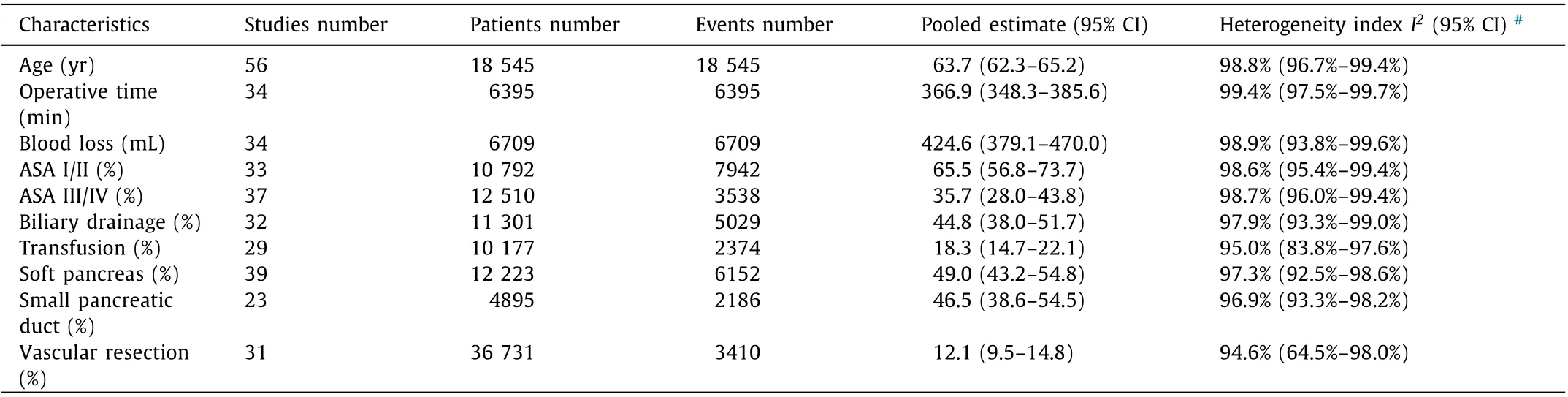
Table 1 Pre- and intraoperative variables in included studies.
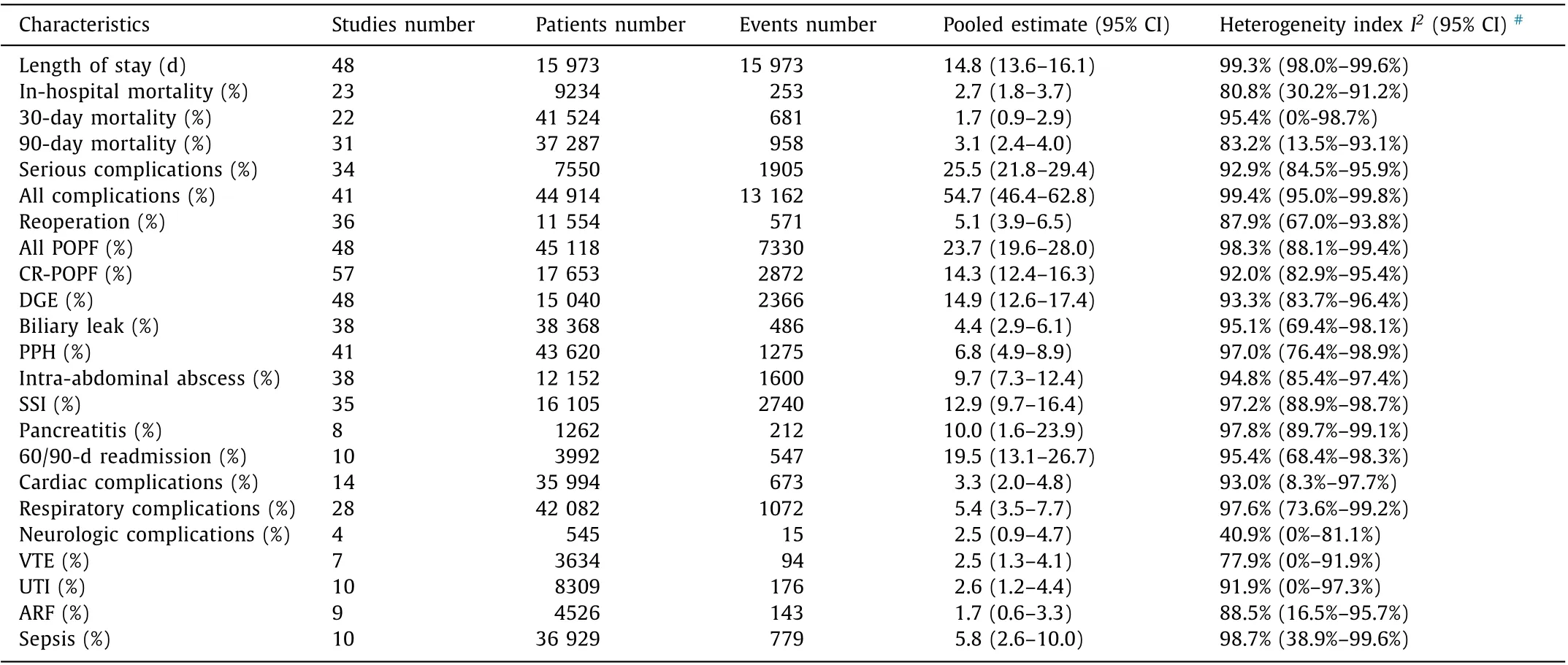
Table 2 Postoperative surgical and medical complications of participants in included studies.
Discussion
To the best of our knowledge, this is the first meta-analysis on modern era PDs, focusing on postoperative complications, including studies with open and minimally invasive PDs, irrespective of reconstruction technique and other patient factors. Both randomized control trials and non-randomized studies were included according to the Cochrane Handbook [15] for systematic reviews addressing adverse effects of interventions. The rationale behind this approach was to avoid possible exclusion of participants that have a priori higher risk of complications. Such participants, as well as patients requiring additional procedures such as vascular resections, will most likely only be included in non-randomized studies.
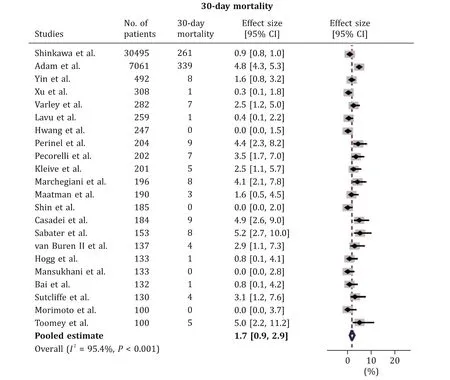
Fig. 2. Forest plot for 30-day mortality. 95% CI: 95% confidence interval.
Notably, the rate of ASA III/IV patients in this meta-analysis is 35.7% which comes in contrast with large registries reporting rates as low as 9% [ 88 , 89 ]. Moreover, a high rate of ASA III/IV (80%) reported from the US is linked with a lower mortality(1.3%) than Germany (5.7%) where ASA III/IV rate of 48% has been reported [88] . This variation is most likely due to different interpretation by doctors or data managers and warrants clarification in future studies. The pooled incidence of overall complications in our study was 54.7%, which is similar to the overall complication rate of 52.9% reported in a recent large retrospective study of 13 110 PDs from the ACS-NSQIP (National Surgical Quality Improvement Program) database in the USA [90] . Serious complications, strictly defined as complications of severity according to Clavien-Dindo ≥III occurred in 25.5% of the patients included in this meta-analysis. This is in agreement with the recent report of 4 large registries of pancreatic surgery of the US and Europe reporting rates between 20.3% and 31.5% [88] . Our pooled 30-day mortality and CR-POPF rates compare favorably to those reported from the ACS-NSQIP database and the transatlantic registries report [ 88 , 90 ]. The multivariate analysis shows that the differences in the rates of CR-POPF can be partially explained by variability in the mean age of patients included in individual studies. Older age is linked with higher rates of pancreatic fistulas [91–93] . Unfortunately, the volume of our data precluded multivariate analysis of other meaningful factors such as sex, ASA class, BMI, neoadjuvant treatment, pancreatic duct size, soft pancreas etc. These variables have reported rates of 10%–90% in individual studies included in our meta-analysis, which represent well recognized risk factors for POPF and account largely for the variability of POPF rates between studies. This is also supported by a recent meta-analysis of risk factors for POPF where the use of a prospective international registry,rather than data from small single or multicenter studies, is recommended in order to define and understand better the variation in practice and to avoid the likelihood of publication bias [94] .
A pooled estimate of 12.1% for vascular resections has been calculated, which is in agreement with the rates reported from a large Japanese and European registries and slightly higher than that reported from the NSQIP database and the Swedish registry( ~19%) [ 88 , 89 , 95 ]. However, the impact of vascular resections on postoperative morbidity and mortality is not clear yet. Data from at least one large study from Asia show no impact on postoperative mortality despite higher intraoperative blood loss and longer operative time but there is also evidence from a USA study showing higher postoperative mortality and morbidity after vascular reconstructions [96] . These results warrant further investigation.
A substantial difference was noted in the length of stay among reports from the USA, Netherlands and our pooled mean (median length of stay of 8 days compared to our pooled mean length of stay of 14.8 days) [88] . A shorter length of stay in centers from North America was also identified in our meta-regression analysis (MD = -6.7 days, compared to studies performed elsewhere).In those reports, shorter hospital stay is associated with higher readmission rates. A recent meta-analysis sets the true benchmark for readmission rate after pancreatic resection between 19% and 20% which matches our pooled estimate (60/90-day readmission of 19.5%) for this variable [97] . In this study, the authors recognize the complex association between center volume and readmission rates.Studies from higher volume centers might report higher, lower or comparable readmission rates because they are more likely to miss readmissions in hospitals outside their emergency care catchment area or because they are more likely to accept more complex and high risk patients from their low volume counterparts or even because they have lower mortality rates; thus more patients at risk for readmission [98] . Readmissions after pancreatic resection are either due to infections or inability to maintain hydration and nutrition and there is evidence that multidisciplinary patient education and post-discharge monitoring can reduce readmissions to more than 50% [99–102] .

Fig. 3. Forest plot for clinically relevant postoperative pancreatic fistula (CR-POPF). 95% CI: 95% confidence interval.
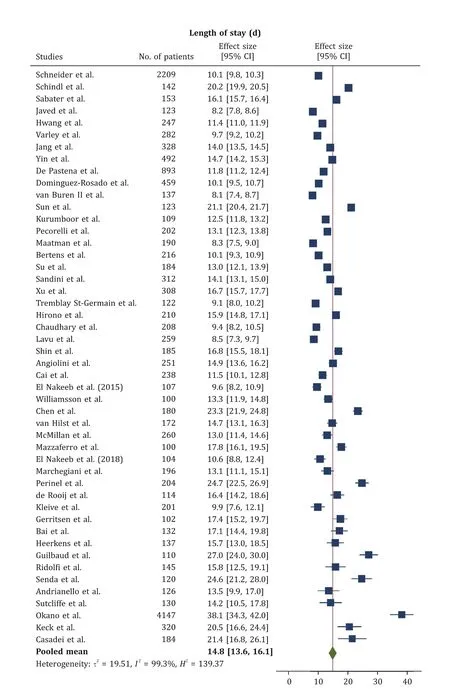
Fig. 4. Forest plot for length of stay. 95% CI: 95% confidence interval.
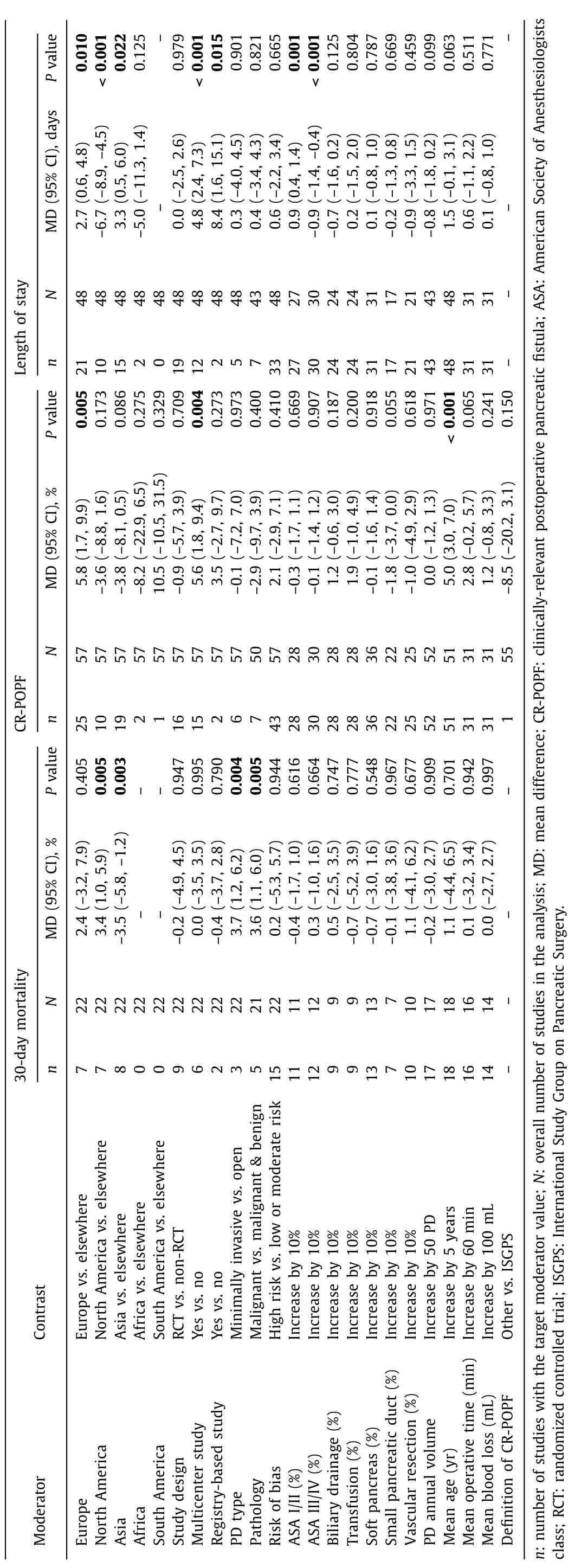
Table 3 Univariate meta-regression analysis investigating study moderators potentially contributing to between-study heterogeneity.
A central theme of the present study was that PD outcomes reported worldwide in the last decade have substantial heterogeneity similar to other major operations such as hepatectomies [103] and esophagectomies [104] . Our results are in line with recent metaanalyses of randomized trials comparing pancreaticogastrostomy versus pancreaticojejunostomy [105] and laparoscopic versus open PD [106] that both showed marked heterogeneity attributed to multiple perioperative factors. Thereby, the pooled rates given in this meta-analysis as indicative of the burden of modern era PD should be interpreted with caution and, in high volume centers,where reliable complication rates can be calculated, it is probably preferable to inform the patients preoperatively about the risks of this procedure based on local data, rather than using heterogeneous results from the literature. Meta-regression showed that European studies reported a higher incidence of overall complications, CR-POPF, DGE, PPH, bile leak, reoperation and longer length of stay and that multicenter studies had higher incidence of serious complications, CR-POPF, DGE and longer length of stay, but a lower incidence of bile leaks. This is perhaps due to the fact that multicenter studies are usually more organized and systematic in reporting complications compared to single-center studies.
Another finding of our study is the wide range of complication definitions which has been stressed out as a problem by another study [107] , which concludes that well-defined outcome parameters in future RCTs are mandatory to reduce heterogeneity [105] . In this systematic review we included studies in which predetermined criteria were used. CR-POPF was used as a main outcome instead of overall POPF incidence, because grade B and C definitions remained almost intact after the 2016 modification by the ISGPS [ 8 , 108 ]. Biochemical leak, on the other hand, is no longer reported as a POPF in recent studies, which may be causing significant variations in overall POPF incidence in the last decade. Moreover, our subgroup analyses by different definitions of complications did not reduce heterogeneity in the reported outcomes. This is probably due to the multifactorial nature of the problem.
Our study has limitations. Although we attempted to explain the observed heterogeneity, its extent limited the generalization of our findings. Because of the relatively small number of primary studies, multivariate meta-regression was deemed unreliable and was not performed for outcomes other than CR-POPF. We were unable to examine if regional differences in the incidences of complications other than CR-POPF that were detected in univariate analyses might be explained by other characteristics of the studies related to the case-mix of the patients included. Moreover, no studies reported whether some patients experienced multiple postoperative complications and it is impossible to know if the overall complication rate involved a summary of multiple complications recorded in a few patients or a true percentage arising from a single complication from each study participant. Risk of bias assessment was performed only at the study level but not at the outcome level. Another limitation is that we arbitrarily chose to include studies involving more than 100 participants, excluding studies reporting outcomes from low-volume pancreatic centers.Finally, due to our strict inclusion criteria, well conducted trials might have been excluded from the meta-analysis despite the fact that they were published during the study period [109] .
In conclusion, this systematic review reported pooled rates of complications after modern PD. Our estimates of complication rates are useful as points of reference for pancreatic units worldwide, regarding the state of contemporary PD today and to inform surgical candidates preoperatively about the potential risks after this major operation. However, this should be done with caution as substantial heterogeneity was observed in reported complication rates and outcomes worldwide.
Acknowledgments
We thank Ms Ruth Monkman for language editing the manuscript.
CRediT authorship contribution statement
Stamatios Kokkinakis: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing.Evangelos I Kritsotakis: Data curation, Formal analysis, Methodology, Writing – review & editing. Neofytos Maliotis: Conceptualization, Data curation, Investigation, Validation. Ioannis Karageorgiou: Conceptualization, Data curation, Investigation, Methodology. Emmanuel Chrysos: Project administration. Konstantinos Lasithiotakis: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources,Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
None.
Ethical approval
Not needed.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi: 10.1016/j.hbpd.2022.04.006 .
 Hepatobiliary & Pancreatic Diseases International2022年6期
Hepatobiliary & Pancreatic Diseases International2022年6期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- YAP activates pancreatic stellate cells and enhances pancreatic fibrosi s
- Combined analysis of imaging tumor capsule with imaging tumor size guides the width of resection margin for solitary hepatocellular carcinoma
- Prediction of early recurrence of hepatocellular carcinoma after liver transplantation based on computed tomography radiomics nomogram
- Technical aspects in pancreaticoduodenectomy and therapeutic strategies for pancreatic cancer: History, current status, and future perspectives
- Contrast-enhanced ultrasound predicts microvascular invasion in patients with hepatocellular carcinoma
- Safety and immunogenicity of COVID-19 vaccination among liver transplant recipients in China
