Combined analysis of imaging tumor capsule with imaging tumor size guides the width of resection margin for solitary hepatocellular carcinoma
Ji-Shuo Cho , Qi Zhu , De-Sheng Chen , Gui-Ming Chen , Xue-Qin Xie , Ai-Qun Liu ,Sen-Lin Zho , Hong-Cheng Sun ,
a Department of General Surgery, Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 20 0 080, China
b Department of Radiology, Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 20 0 080, China
c Department of Colorectal Surgery, Fudan University Shanghai Cancer Center, Shanghai 20 0 032, China
Keywords:Hepatocellular carcinoma Resection Hepatectomy Magnetic resonance imaging Preoperative imaging
A B S T R A C T
Introduction
Hepatocellular carcinoma (HCC), the major subtype of liver cancer, is a global medical issue that causes high morbidity and mortality. Surgical interventions are the mainstay treatments for HCC, among which hepatectomy is preferred for patients with resectable HCC [1] . Successful hepatectomy requires complete removal of the tumors and preservation of adequate remnant liver,both of which are closely associated with the width of resection margin (RM), an essential surgical factor that can be controlled by surgeons. Nevertheless, debates still exist regarding the optimal width of RM. Wide RM has been reported to reduce the incidence of postoperative HCC recurrence, contributing to a favorable prognosis [2–6] . Inconsistently, other studies demonstrated comparable prognoses between HCC patients with narrow RM and wide RM [7–9] . Moreover, patients with wide RM experienced worse perioperative outcomes and more surgical complications, especially those with underlying liver disease [8] .These controversial findings may be mainly rooted in the different probabilities of existing residual tumor cells in the remnant liver after hepatectomy. Therefore, it is advisable to set different RM widths for HCC patients with different probabilities of tumor recurrence.
Tumor capsules can gradually form as HCC grows, which is a unique feature of progressed HCC [10] . Encapsulated HCCs exhibit a much lower incidence of direct invasion, venous permeation, and satellite lesions than nonencapsulated tumors [ 11 , 12 ].Moreover, complete tumor encapsulation is an independent predictor of favorable prognosis for HCC patients [ 4 , 13 , 14 ]. Dynamic contrast-enhanced magnetic resonance imaging (MRI) and computed tomography (CT) have been widely used for the detection of liver tumors. Compared to CT, MRI is more sensitive and accurate in characterizing HCCs and identifying tumor capsules [15] .In addition, high consistency has been reported between the tumor capsule on preoperative MRI and pathological findings after hepatectomy [16–18] . In this study, we aimed to investigate whether the imaging tumor capsule (ITC) on MRI could represent a prognostic predictor for HCC patients receiving hepatectomy, and elucidate whether ITC combined with imaging tumor size (ITS)could guide RM width for those patients.
Patients and methods
Study cohort
A total of 386 consecutive patients who underwent hepatectomy with pathologically confirmed HCC from January 2013 to July 2019 in our center were retrospectively reviewed. The exclusion criteria were as follows: (i) prior application of transarterial chemoembolization (TACE), radiofrequency ablation (RFA) or other anticancer therapies; (ii) recurrent HCC or ruptured HCC; (iii)palliative resection; (iv) death within a month or loss of followup within three months after surgery; (v) multiple tumors identified by preoperative CT/MRI and/or intraoperative ultrasound; (vi)missing data on preoperative MRI. This study was approved by the Medical Ethics Committee of Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine and was registered at http://www.chictr.org (ChiCTR20 0 0 032962). Informed consent was obtained from each participant.
Data collection and definitions
Patient clinicopathological data were extracted from the electronic record system of our hospital. The information included demographics, routine laboratory tests, serum tumor markers, hepatitis serology, preoperative MRI findings, surgery-related variables and pathological reports. The neutrophil-to-lymphocyte ratio (NLR)was calculated as the neutrophil count divided by the lymphocyte count. Contrast-enhanced MRI was performed within one week before surgery. ITC was evaluated qualitatively according to the following criteria: an enhancing high-signal-intensity rim on the portal- or delayed-phase T1-weighted images and/or a low-signalintensity rim on T1-weighted and T2-weighted images [ 19 , 20 ]. MRI images were independently reviewed by two senior radiologists,who had no prior knowledge of clinical data. After a comprehensive review of all the available images, ITC was categorized as follows: (i) complete ITC: tumor capsules surround the entire tumor circumference. When a tumor displays exophytic growth, the protruding part should be completely encapsulated and in line with the capsules of the main tumor; (ii) incomplete ITC: a portion of the tumor is not covered by the tumor capsules, or discernible tumor capsules cannot be found around the tumor. ITS was defined as the longest tumor diameter presented on MRI. The RM width reported by pathologists was defined as the shortest distance from the tumor edge to the RM of the parenchyma. A cutoff value of 5 mm for the RM width was set to subdivide patients into two groups, including the narrow RM group ( < 5 mm) and the wide RM group ( ≥5 mm), as suggested by previous reports [ 2 , 8 , 9 , 21 ].
Postoperative follow-up
Patients were followed up at the outpatient clinic after discharge according to the standard protocol of our center. Tumor recurrence was monitored by serum alpha-fetoprotein (AFP) and/or des-γ-carboxy prothrombin, abdominal ultrasonography, chest CT,and enhanced CT/MRI (every three months for the first two years and every six months for the following years after surgery). Postoperative HCC recurrence was defined as the detection of new neoplastic lesions in the liver or extrahepatic organs (lung, adrenal glands, bone, etc.) after exclusion of primary cancers. When HCC recurrence was suspected, positron emission tomography and radioisotope bone scans were scheduled if necessary, in addition to regular imaging examinations. Ultrasound/CT-guided tissue biopsy was implemented when the diagnosis of HCC recurrence was in doubt. Elevated levels of serum tumor markers were not a prerequisite for the diagnosis of HCC recurrence, but progressive elevation was considered HCC recurrence even without definite neoplastic lesions. A consensus on newly diagnosed HCC recurrence was reached by a panel of experts including radiologists and surgeons. RM recurrence was defined as intrahepatic recurrence located within 1 cm from the RM, regardless of simultaneous recurrence at other sites. Most recurrent patients were treated with a multidisciplinary treatment program including TACE, RFA, resection, liver transplantation, and/or sorafenib. Some patients did not receive any aggressive treatment for tumor relapse due to highly advanced HCC accompanied by poor physical status. The last follow-up date was 1st July 2020. Recurrence-free survival (RFS)was defined as the period from the date of hepatectomy to the date of HCC recurrence or last follow-up. Overall survival (OS) was defined as the period from the date of hepatectomy to the date of either death or last follow-up.
Statistical analysis
Continuous variables were presented as median and interquartile range and were compared by Mann-WhitneyUtest. Categorical variables were presented as frequencies and percentages and were compared using Chi-square test or Fisher’s exact test as appropriate. Survival analyses were performed using Kaplan-Meier method and were compared by log-rank test. Subgroup analyses based on ITS were conducted to evaluate the impact of ITC on prognosis.Univariate and multivariate Cox regression analyses were used to identify independent risk factors. Variables withP< 0.1 in univariate analysis were further included in the multivariate analysis.AP< 0.05 was considered statically significant. Statistical analyses were performed using SPSS version 24 (IBM, Armonk, New York,USA).
Results
ITC and ITS were independent prognostic predictors for patients with solitary HCC
After execution of the exclusion criteria, a total of 247 patients with solitary HCC were included in this study ( Fig. 1 ). The median follow-up time was 44.5 months. Seventy-two patients (29.1%)died during follow-up. One hundred and four patients (42.1%) experienced tumor recurrence. The 1-, 2-, 3-, and 5-year RFS rates were 75.6%, 66.8%, 58.1%, and 53.5%, respectively. The 1-, 2-, 3-,and 5-year OS rates were 90.2%, 79.4%, 73.5%, and 63.8%, respectively.
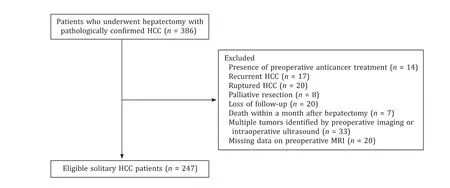
Fig. 1. Flow chart of this study. HCC: hepatocellular carcinoma; MRI: magnetic resonance imaging.
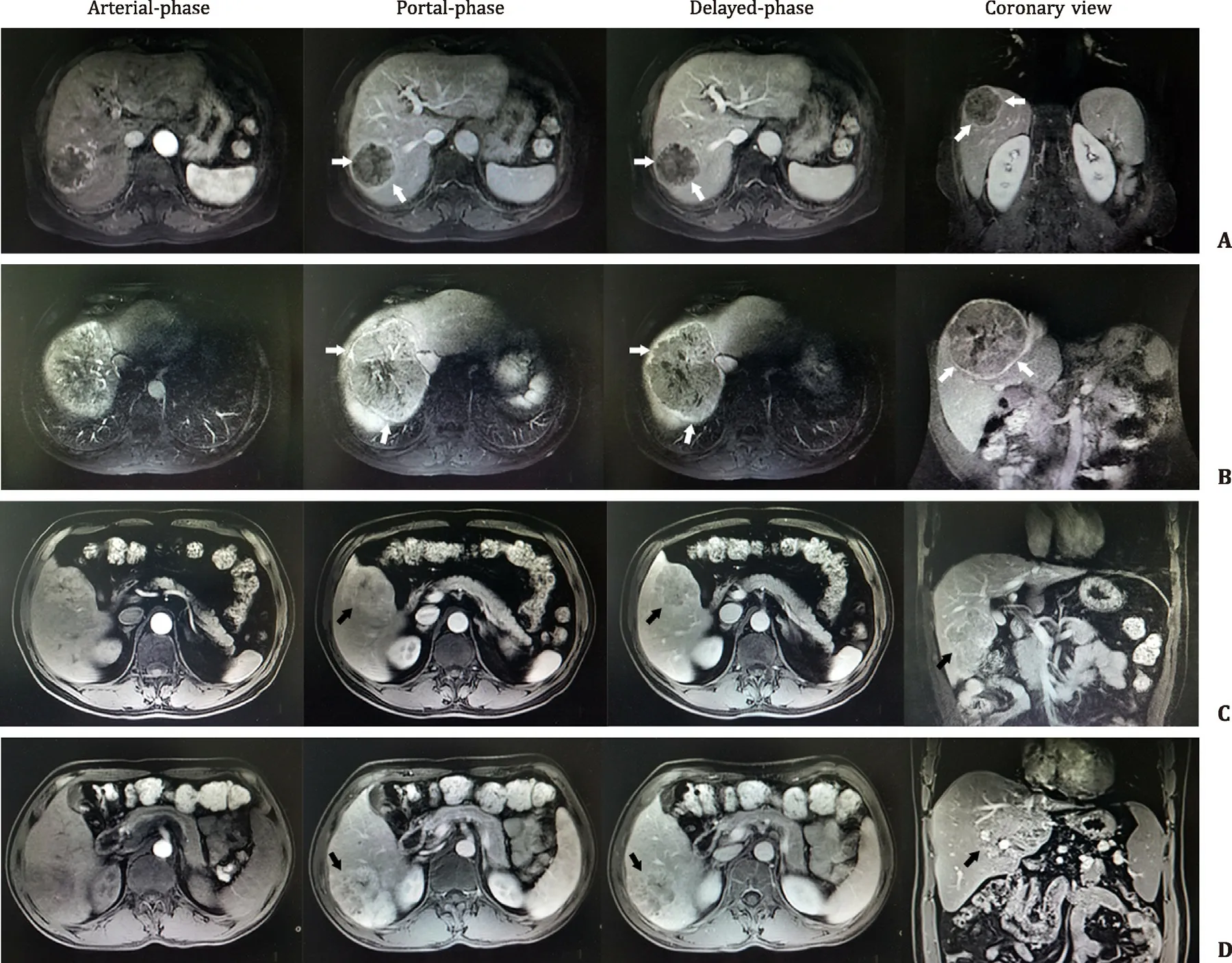
Fig. 2. Representative MRI images of complete ITC ( A , B ) and incomplete ITC ( C , D ). From left to right, the images of each row are typical MRI images of arterial-phase,portal-phase, delayed-phase, and coronary view. The white arrows point to tumor capsules, and the black arrows indicate the portions without coverage of tumor capsules.ITC: imaging tumor capsule; MRI: magnetic resonance imaging.
Representative MRI images of different ITC statuses were shown in Fig. 2 . In our cohort, 126 patients (51.0%) had complete ITC,and 121 (49.0%) showed incomplete ITC. Patients with complete ITC had a better tumor differentiation status (well or moderately differentiated tumor 87.3% vs. 76.9%,P= 0.032) and a lower incidence of microvascular invasion (MVI) (40.2% vs. 57.9%,P= 0.014)compared with those with incomplete ITC ( Table 1 ). In addition,the patients with complete ITC had better RFS and OS than those with incomplete ITC (bothP< 0.001; Fig. 3 A, B). Univariate Cox analysis revealed that ITC was significantly associated with RFS and OS, along with other available preoperative parameters (Table S1). Multivariate Cox analysis demonstrated that incomplete ITC adversely influenced patient prognosis [hazard ratio (HR) = 2.061,P= 0.001 for RFS; HR = 2.169,P= 0.005 for OS; Table 2 ]. Moreover, ITS > 3 cm, AFP > 400 ng/mL, and albumin < 35 g/L were independently associated with dismal RFS and OS ( Table 2 ).
ITS-based subgroup analyses to evaluate the prognostic impact of ITC
We set different ITSs (2 cm, 3 cm, 4 cm, and 5 cm) as the cutoff values of dichotomous analysis on patient prognosis. We found that 3 cm, 4 cm, and 5 cm could significantly differentiate patient subgroups with different outcomes, whereas 2 cm could not (Fig. S1). We finally chose 3 cm as the cutoff valuerather than 4 cm or 5 cm based on the following reasons: (i) ITC showed the weakest prognostic influence on patients with ITS ≤3 cm ( Fig. 3 C, D) compared with those with ITS ≤4 cm or ≤5 cm (Fig. S2); (ii) the stratification efficacy of ITC on the patients with ITS > 3 cm was significant (P< 0.001; Fig. 3 E, F).In the patients with ITS ≤3 cm, the prognosis of the complete ITC subgroup was comparable to that of the incomplete ITC subgroup (P= 0.599 for RFS;P= 0.505 for OS; Fig. 3 C, D). Among patients with ITS > 3 cm, those with complete ITC displayed better RFS and OS than those with incomplete ITC (bothP< 0.001;Fig. 3 E, F).
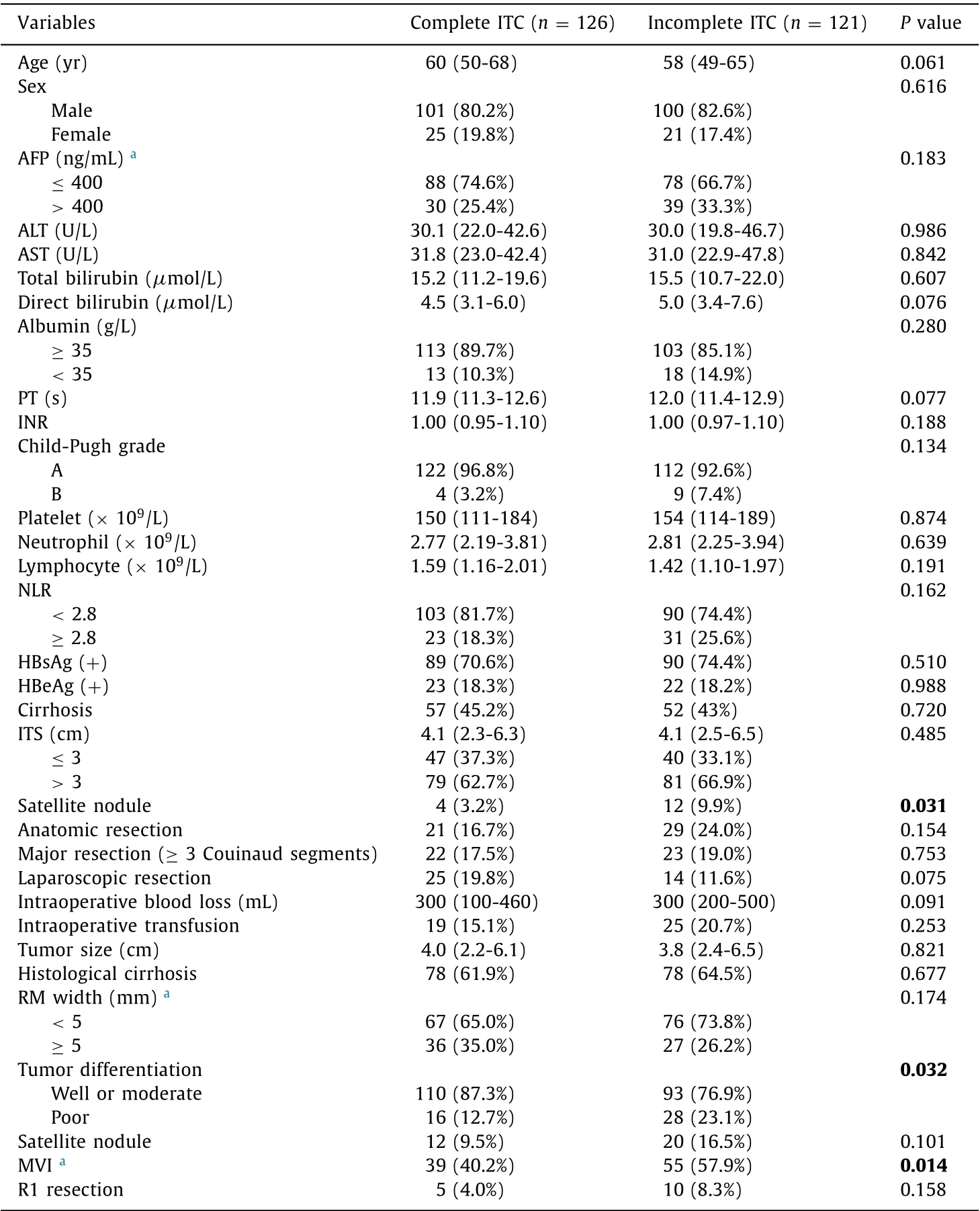
Table 1.Baseline clinicopathological features of the entire cohort subdivided by ITC status.
Combining ITC and ITS as stratification factors to evaluate the impact of RM width on prognosis and RM recurrence
We excluded 41 patients in further RM-related subgroup analysis due to missing data on RM width. In the entire cohort, the wide RM group showed improved RFS and OS compared with the narrow RM group, but the improvement was not significant (P= 0.075 andP= 0.067; Fig. 4 A, B). The incidence of RM recurrence was higher in the narrow RM group compared with the wide RM group(24.2% vs. 6.9%,P= 0.005; Table 3 ). In patients with ITS ≤3 cm, comparable RFS and OS were observed between the wide RM group and the narrow RM group (P= 0.733 andP= 0.841; Fig. 4 C,D), and the incidence of RM recurrence was also comparable between the two groups (15.6% vs. 4.3%,P= 0.337; Table 3 ). In patients with ITS > 3 cm, the wide RM group showed better RFS and OS compared with the narrow RM group (P= 0.039 andP= 0.036;Fig. 4 E, F). Next, we subdivided the patients with ITS > 3 cm according to their ITC statuses. Baseline characteristics between patients with wide RM and those with narrow RM were comparable in the complete ITC subgroup as well as in the incomplete ITC subgroup (Table S2). In patients with ITS > 3 cm and complete ITC, no difference in prognosis was noted between the wide RM group and the narrow RM group (P= 0.606 for RFS;P= 0.916 for OS; Fig. 4 G,H), and the incidence of RM recurrence was similar between the two groups (17.5% vs. 9.5%,P= 0.649; Table 3 ). However, in patients with ITS > 3 cm and incomplete ITC, the wide RM group showed better RFS and OS than the narrow RM group (P= 0.037 andP= 0.018; Fig. 4 I, J), and the wide RM group demonstrated a lower incidence of RM recurrence than the narrow RM group(7.1% vs. 41.0%,P= 0.046; Table 3 ). Cox regression analysis was performed for patients with ITS > 3 cm and incomplete ITC, and wide RM was revealed as a favorable prognostic factor for both RFS and OS in univariate analysis (Table S3), and was an independent protective factor in multivariate analysis (HR = 0.298,P= 0.013 for RFS; HR = 0.327,P= 0.047 for OS; Table 4 ).
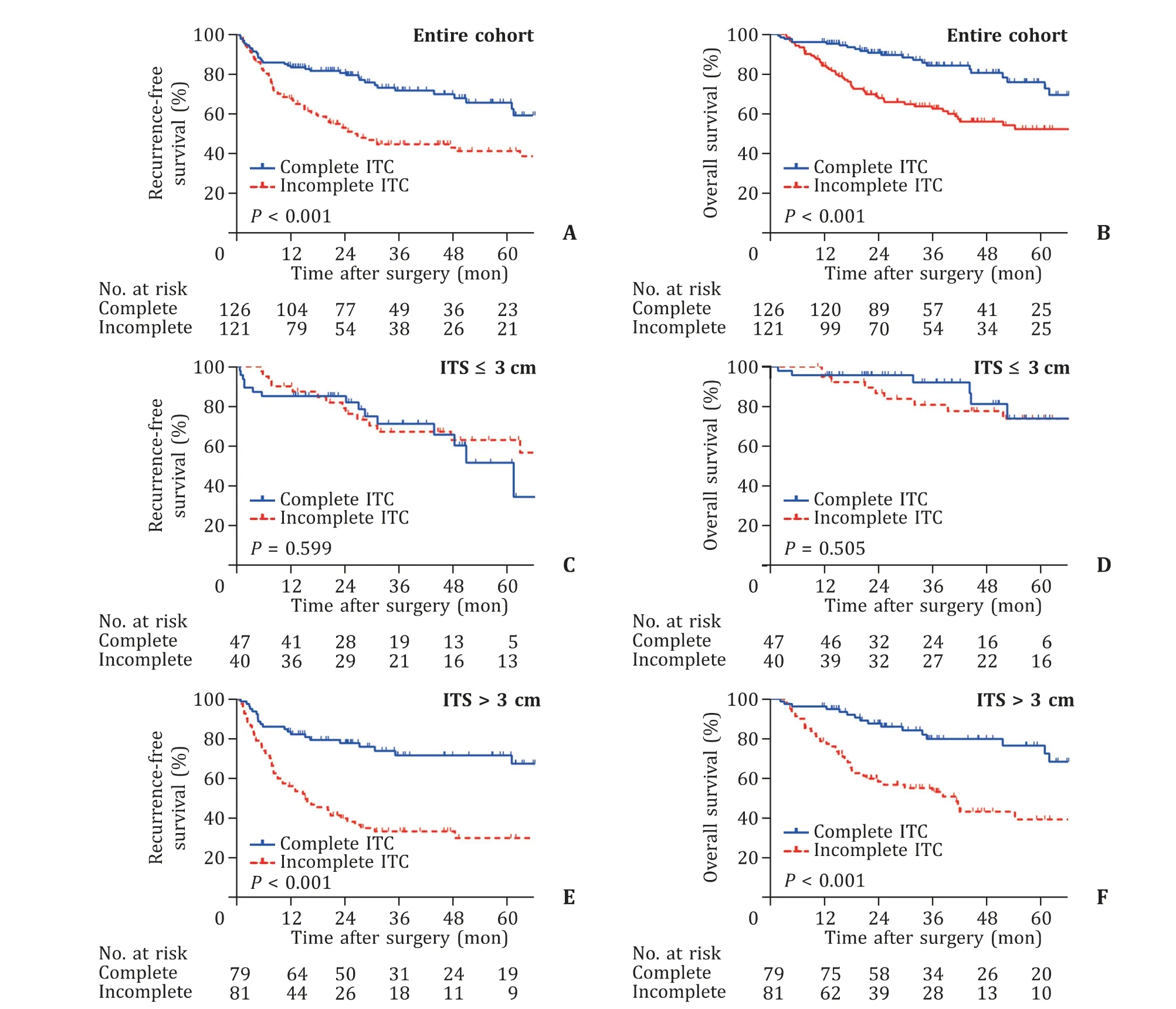
Fig. 3. Survival outcomes of the entire cohort and ITS-based subgroups divided by ITC status. Recurrence-free survival and overall survival curves for the entire cohort ( A ,B ), patients with ITS ≤3 cm ( C , D ), and those with ITS > 3 cm ( E , F ) divided by ITC status. ITS: imaging tumor size; ITC: imaging tumor capsule.
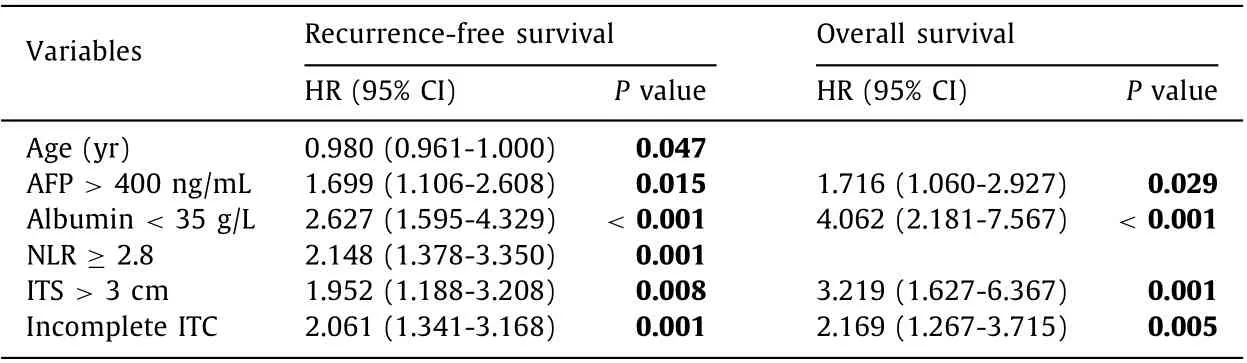
Table 2.Multivariate Cox analysis of preoperative risk factors for recurrence-free survival and overall survival in the entire cohort.
Discussion
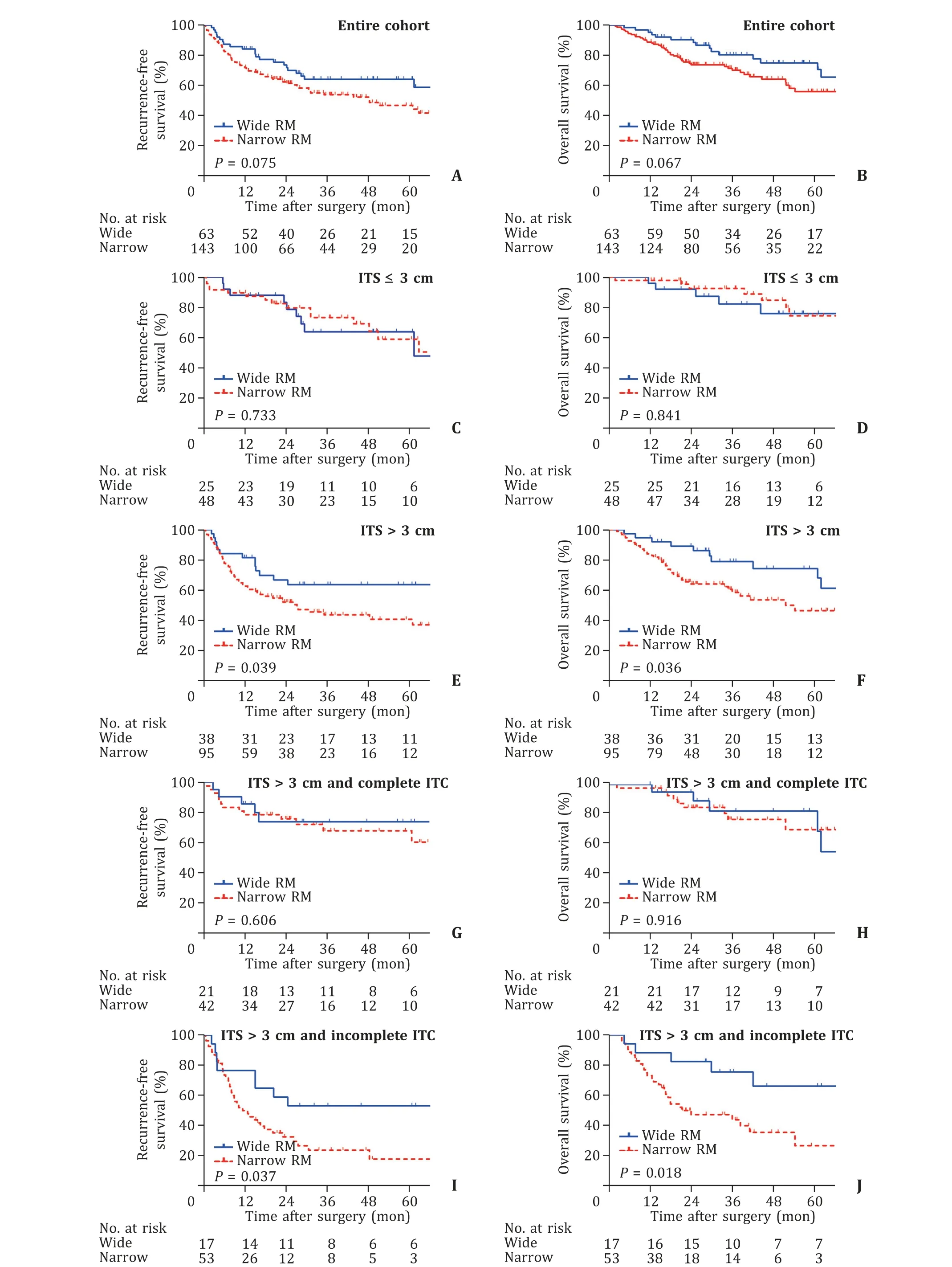
Fig. 4. Survival outcomes of ITS-based subgroups divided by RM width. Recurrence-free survival and overall survival curves for the entire cohort ( A , B ), patients with ITS ≤3 cm ( C , D ), those with ITS > 3 cm ( E , F ), those with ITS > 3 cm and complete ITC ( G , H ), and those with ITS > 3 cm and incomplete ITC ( I , J ) divided by RM width. ITS:
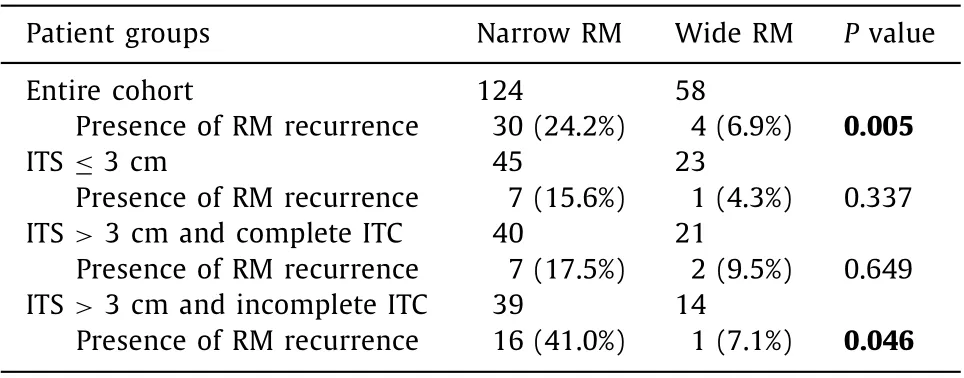
Table 3.The influence of RM width on the incidence of RM recurrence in the entire cohort and its subgroups ( n = 182 ?).
The principles of hepatectomy for HCC patients include radical resection and surgical safety, both of which are closely related to the width of RM. Wide RM is thought to be conducive to radical resection of HCC and thus contributes to reducing the risk of surgery-related tumor recurrence [6]. In clinical practice,however, wide-margin resection for HCC, particularly large tumors,is occasionally infeasible due to anatomical limitations or insuffi-cient remnant liver. Recent data from an international multicenter study demonstrated that tumor recurrence patterns, including RM recurrence and the 2-year recurrence rate, were similar between HCC patients with wide RM and narrow RM [5] . It has been proposed that HCC recurrence after hepatectomy is mostly attributed to venous dissemination, a procedure that wide-margin resection cannot prohibit [7] . Moreover, wide RM could result in more frequent blood transfusion, more postoperative complications, and higher in-hospital mortality rates, especially in patients with cirrhotic backgrounds [8] . The optimal width of RM remains under fierce debate leaving hepatic surgeons in an academic dilemma,which highlights the necessity to differentiate between patients who may benefit from wide RM and those who may not. Theoretically, extending the RM width may benefit patients whose tumor cells tend to invade beyond their primary lesion. A previous study reported that wide RM could reduce early recurrence in patients with MVI, but not in those without MVI [13] . Nevertheless,accurate assessment of MVI before surgery is particularly difficult;thus, MVI is not a desirable candidate marker for the guidance of RM width. Tumor size has been reported as a stratification factor for identifying patients who might benefit from wide RM. HCC patients with RM ≥1 cm were revealed to have better RFS than those with RM < 1 cm when tumor size ≤5 cm, but no survival difference was observed when tumor size > 5 cm [5] . Another study demonstrated that patients with RM ≥1 cm exhibited superior RFS compared with those with RM < 1 cm only when the tumor size ranged from 2 to 5 cm [22] . Similar results were reported by a prospective trial in which wide RM marginally improved the RFS of patients with tumor sizes ranging from 2 to 5 cm (P= 0.08) [6] .However, Poon et al. [7] stratified patients based on tumor size ( ≤5 cm and > 5 cm) and found no significant correlation between RM width and the 5-year recurrence rate in either subgroup. These inconsistent results indicated low reliability of tumor size as the sole stratification factor for guiding RM width.
In this study, the Cox regression analysis for the entire cohort only included preoperative factors, in that these parameters were available before hepatectomy and could be useful in making surgical strategies concerning the RM width. Complete ITC was identified as an independent predictor for favorable RFS and OS in the entire cohort. Complete ITC was closely associated with better tumor differentiation and a lower incidence of MVI, indicating that complete ITC may represent favorable biological features of HCC and prevent tumor cells from escaping from the primary site. In addition to ITC, ITS ( ≤3 cm/ > 3 cm) was another independent prognostic predictor of the entire cohort. In the ITS ≤3 cm subgroup, neither ITC nor RM width impacted prognosis, which can be explained by the fact that small HCCs are less likely to develop tumor capsules than large HCCs [ 10 , 19 ] and that small HCC patients commonly have decent prognosis after radical resection regardless of RM width. In addition, the incidence of RM recurrence was similar between the narrow RM and wide RM groups, suggesting that narrow RM did not increase the risk of RM recurrence in patients with ITS ≤3 cm. Therefore, extending RM width may have limited prognostic value in the ITS ≤3 cm subgroup. In the patients with ITS > 3 cm and complete ITC, the narrow RM group showed excellent outcomes comparable to the wide RM group,and the incidence of RM recurrence was also comparable between the two groups. Namely, it is unnecessary to perform widemargin resection for patients with complete ITC because wide RM does not offer survival benefits but increases the complexity of surgery and the incidence of liver failure. Our results were consistent with a previous report that hepatectomy along tumor capsules could obtain a “clear” margin and achieve satisfactory therapeutic effects [23] . Therefore, we proposed that complete ITC might represent a preoperative marker to select patients who are suitable for narrow-margin resection when their ITS > 3 cm. In patients with ITS > 3 cm and incomplete ITC, the prognosis of the wide RM group was superior to that of the narrow RM group, and RM width was verified to be an independent prognostic factor. In addition, the incidence of RM recurrence was lower in the wide RM group than in the narrow RM group. Therefore, wide RM should be industriously pursued in patients with ITS > 3 cm and incomplete ITC due to its conspicuous protective effect. However, in the case of large tumors and insufficient remnant liver, neoadjuvant therapies are occasionally needed to downsize HCC to achieve wide RM.
Although the present study provided a novel strategy for the guidance of hepatectomy regarding RM width, it did have certain limitations. Firstly, the RM width in this study referred to the final RM width recorded in pathological reports instead of the intended RM width during surgery, because the intended RM width was unavailable due to the retrospective nature of our study. Considering that the final RM width is not equal to the intended RM width,multicenter prospective studies are required to further validate our results. Secondly, patients with multiple HCCs identified by pre-operative imaging and/or intraoperative ultrasound were excluded from the analysis due to the difficulty in ITC assessment, because different nodules of a patient may display diverse ITC statuses. Further analyses are needed to evaluate whether other preoperative factors would help guide RM width for patients with multiple nodules.
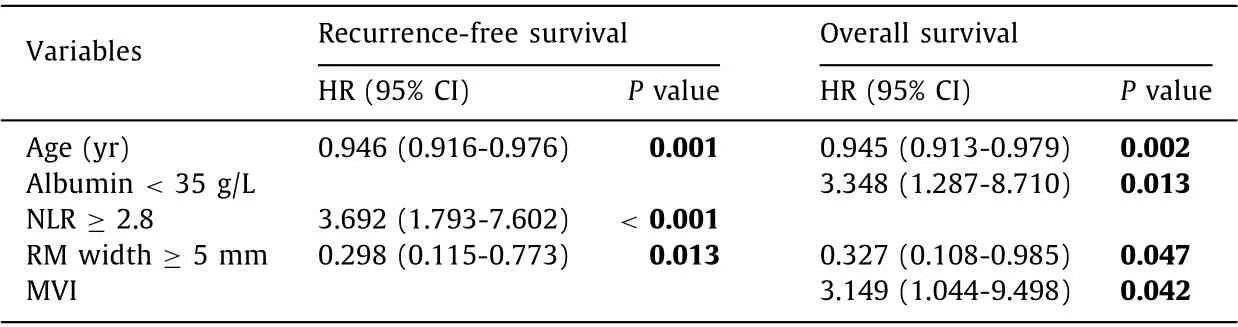
Table 4.Multivariate Cox analysis of risk factors for recurrence-free survival and overall survival in patients with ITS > 3 cm and incomplete ITC.
In conclusion, MRI-based ITC and ITS are independent prognostic predictors for patients with solitary HCC who received hepatectomy. Combined analysis of ITC with ITS provides a convenient decision-making tool for instructing RM width. HCC patients with ITS ≤3 cm regardless of ITC status and those with ITS > 3 cm and complete ITC are indeed fit to receive narrow-margin resection without any compromise in prognosis. In contrast, wide RM is highly recommended for those with ITS > 3 cm and incomplete ITC. Therefore, we advise hepatic surgeons to focus on ITC and ITS to develop a safe and sensible surgical strategy for HCC patients.
Acknowledgments
We thank Dr. Chun-Xiao Wu from Shanghai Municipal Center for Diseases Control and Prevention for his sincere assistance in patient follow-up.
CRediT authorship contribution statement
Jia-Shuo Chao: Data curation, Formal analysis, Writing - original draft. Qi Zhu: Data curation, Investigation, Methodology, Visualization. De-Sheng Chen: Data curation, Investigation, Methodology, Validation. Gui-Ming Chen: Resources, Supervision. Xue-Qian Xie: Data curation, Software. Ai-Qun Liu: Data curation, Software.Sen-Lin Zhao: Conceptualization, Project administration. Hong-Cheng Sun: Conceptualization, Funding acquisition, Supervision,Writing - review & editing.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81672846) and the Clinical Research Innovation Plan of Shanghai General Hospital (CTCCR-2019C08).
Ethical approval
The study was approved by the Medical Ethics Committee of Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine (2020K038). Written informed consent was obtained from all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.hbpd.2021.12.009 .
 Hepatobiliary & Pancreatic Diseases International2022年6期
Hepatobiliary & Pancreatic Diseases International2022年6期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- YAP activates pancreatic stellate cells and enhances pancreatic fibrosi s
- Prediction of early recurrence of hepatocellular carcinoma after liver transplantation based on computed tomography radiomics nomogram
- Complications of modern pancreaticoduodenectomy: A systematic review and meta-analysis
- Technical aspects in pancreaticoduodenectomy and therapeutic strategies for pancreatic cancer: History, current status, and future perspectives
- Contrast-enhanced ultrasound predicts microvascular invasion in patients with hepatocellular carcinoma
- Safety and immunogenicity of COVID-19 vaccination among liver transplant recipients in China
