Dengue hemorrhagic fever with rectus sheath hematoma: A case report
Boudhayan Bhattacharjee,Hardik Patel,Rucha Karad,Vasireddy Teja,Agnibho Mondal,Soumendra Nath Haldar,Bibhuti Saha
Department of Infectious Diseases and Advanced Microbiology,School of Tropical Medicine,Kolkata,India
ABSTRACT Rationale: Acute pain is a medical emergency that requires prompt abdominal evaluation and management.Dengue,a mosquitoborne arboviral infection,can lead to complications such as acute abdominal pain.Patient concerns: A 72-year-old hypertensive female presented with high-grade intermittent fever with chills and rigors for four days.She was diagnosed with dengue fever (NS1Ag-reactive) the day before admission.A contrast-enhanced computed tomography of the abdomen showed a hematoma along the rectus sheath which was managed conservatively as per surgical opinion.Diagnosis: Dengue hemorrhagic fever with rectus sheath hematoma.Interventions: Blood transfusion and fluid therapy.Outcomes: Ten days after discharge,the patient reproted no pain in the right iliac fossa and the size of the hematoma was significantly reduced.Lessons: Although it is rarely seen as a cause of acute abdomen,complaints of adnominal pain should never be ignored in critical or convalescent phase of dengue fever.Radiological investigations should be promptly conducted as hematoma is often difficult to be diagnosed clinically.Delay in diagnosis of rectus sheath hematoma can be fatal.
KEYWORDS: Dengue fever;Rectus sheath hematoma;Surgical emergency;Acute appendicitis
1.Introduction
Dengue is a mosquito-transmitted arboviral infection,which has become a disease of public health concern globally.It usually presents as fever with myalgia and body ache,worsen by bleeding,shock,or organ involvement.Majority of patients present with fever,flulike symptoms,constitutional symptoms,and some forms of plasma leakage.However,reports of dengue cases with organ involvement in the form of hepatitis,kidney injury,myocarditis,encephalitis,pancreatitis,acute respiratory distress syndrome are on the rise and this is called expanded dengue syndrome[1].Dengue hemorrhagic fever (DHF) is the severe form,characterised by increased vascular permeability leading to plasma leak and increased hemorrhagic chances.The increased vascular permeability is usually short-lived and involves plasma leaking into peritoneal spaces (the pleural cavity and tissue plains called third spaces)[1].Dengue fever is usually manged with intravenous fluids and other supportive therapy.In severe thrombocytopenia or bleeding usually platelets and packed red cells are transfused[1].It has been observed that majority (81%) of the cases were haemodynamically stable with no severe symptoms;another 15% cases were mild and required treatment in primary healthcare;while 0.3% cases showed severe signs of DHF or dengue shock syndrome.About 1% hospitalised patients required blood transfusion.There has been reports of spontaneous bleeding in different parts of body,but spontaneous bleeding into rectus muscle leading to haematoma formation is rare[2].
We report a case of dengue hemorrhagic fever with spontaneous rectus sheath haematoma.The patient presented as severe right iliac fossa pain mimicking acute appendicitis.The patient was manged promptly with radiological evaluation for early diagnosis and subsequently was managed conservatively.This case adds to our existing knowledge that rectus muscle hematoma is one of the rare of complications of dengue hemorrhagic fever.
2.Case presentation
Informed consent was obtained from the patient for the publication of this case report and any accompanying images.
A 72-year-old hypertensive female from Kolkata,West Bengal,India,presented with high-grade intermittent fever with chills and rigors for the last four days.She also had severe muscle pain,body ache,nausea,and vomiting associated with fever.She was unable to eat or drink due to the illness.She was on telmisartan 40 mg and hydrochlorothiazide 12.5 mg for control of hypertension.She was diagnosed to have dengue fever (NS1Ag -Reactive) on the day before admission.At admission,she was dehydrated,mild pallor,BP-110/70 mmHg,pulse-122/min,temperature-38.9 ℃,SpO2-98%at room air,alert,co-operative,bilateral vesicular breath sounds in the chest,CVS-S1,S2 audible,Tender 2 cm hepatomegaly below right costal margin,no free fluid.Immediately she was put on Ⅳ fluids (volume calculated according to Holliday-Segar formula),antiemetics,and other supportive therapies.On laboratory examination,she had low platelets,low haemoglobin and low total leucocyte counts,with raised liver enzymes.On day 3 of illness,she had a significant drop of haematocrit with low blood pressure(90/60 mmHg).Then,she was immediately transfused with packed red blood cells.Her blood culture,urine cultures were showing no growth.After the initial hypotension and drop in haematocrit,she continued to have low haemoglobin (7-8 g/dL) with normal blood pressure (without antihypertensives).On the 9th day of illness,she had severe right iliac fossa pain mimicking acute appendicitis with continued nausea,while there was no history of trauma during this period.And the stool occult blood test was strongly positive.Intravenous fluids,ceftriaxone,intravenous metronidazole and other supportive therapies were used to relieve her abdominal pain.On day 13 of illness contrast-enhanced computed tomography of the abdomen showed a soft tissue lesion in the right lower abdomen suggestive of rectus muscle hematoma (Figure 1).Antibiotics were discontinued when her total leucocyte and temperature got normal.After 2-3 days of conservative management,she was stable with a mild tender right iliac fossa mass.The patient was discharged on day 14 of illness with an advice to do a follow-up ultrasonography after 15 days.Ten days past discharge,she had no pain in the right iliac fossa and the size of the hematoma was significantly reduced (from 11 cm×3 cm to 4 cm×2 cm) on sonography.After 15 days after discharge,she had no right iliac fossa pain or mass.Ultrasonography also shown minimal hematoma at day 15 post-discharge.
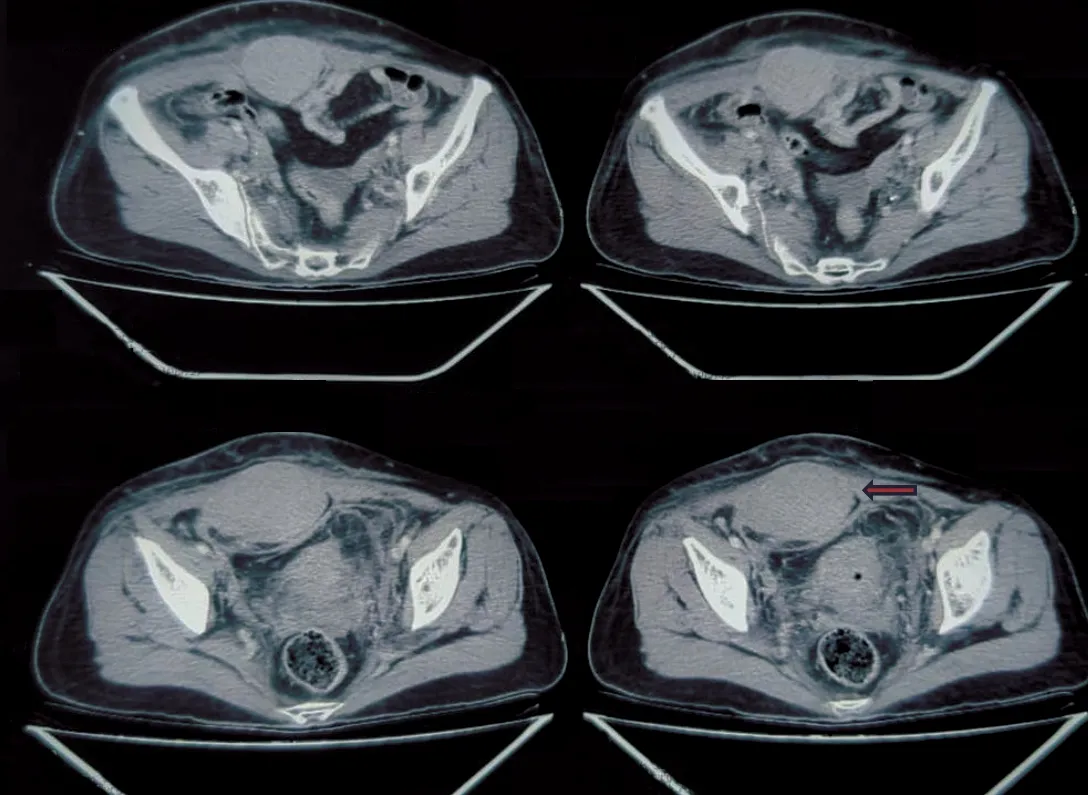
Figure 1.Contrast-enhanced computed tomographic scan of the abdomen of a 72-year-old female who had dengue hemorrhagic fever with rectus sheath hematoma.The arrow indicates a rectus muscle hematoma.
3.Discussion
Rectus sheath hematoma (RSH) usually presents as bleeding within the rectus abdominis muscle sheath.This is commonly caused by ruptured epigastric vessels or a tear of the rectus muscle[3].Usual known risk factors of spontaneous RSH are female sex,pregnancy,obesity,anticoagulant drugs,abdominal straining,severe vomiting,and intractable cough[4].Complications in patients with DHF present with bleeding,usually result from the combination of thrombocytopenia,increased vascular fragility,increased fibrinolysis,pro-coagulation and anticoagulation factors imbalance.In critical stage of DHF,there is defervescence of fever and higher degree of plasma leakage and low platelet count,which in some cases may lead to circulatory failure or bleeding into vital organs[5].
RSH can be divided by the severity of haemorrhage as seen on CT scan.Type-Ⅰ RSH are one-sided hematomas contained only within the muscle.Type-Ⅱ RSH is bilateral hematoma/hematomas not contained within the muscle sheath.Type-Ⅲ RSH is called when blood enters the pre-vesicular space or peritoneum.Usually type Ⅰ&Ⅱ RSH can be managed conservatively,but type Ⅲ usually needs surgery.Treatment of spontaneous RSH is generally conservative including resuscitation,correction of coagulopathy,analgesia,and treatment of the underlying condition[6].Interventional radiological intervention and embolization is preferred in cases of continued bleeding with surgery being considered as the last option[7].RSH has been mistaken for many acute abdominal diseases like acute appendicitis,dissecting abdominal aneurysm,cholecystitis and biliary colic,cholelithiasis,diverticular disease,peptic ulcer disease,acute gastritis and obstructed intestinal hernias.Our case mimicked acute appendicitis and managed conservatively with Ⅳ fluids,analgesics and blood transfusion as it fits into RSH type Ⅱ.
4.Conclusions
Management of spontaneous RSH is generally conservative including resuscitation,correction of coagulopathy,analgesia,and treatment of the underlying condition.It is important to be vigilant while treating patients who present with abdominal pain or any neuro-deficit during the convalescent phase of dengue fever,as it could be a presenting symptom of spontaneous hematoma in different parts of the body.Prompt imaging in relevant areas could make the diagnosis and father treatment possible,otherwise,it could lead to a fatal outcome.This case report emphasises that during dengue treatment especially in critical or convalescent phase,complains of adnominal pain should never be ignored.It should set an alarm to investigate radiologically because it is often difficult to judge these complications like hematoma clinically,while prompt action could ensue a proper treatment of the complication.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This case report did not receive any specific grants from funding agencies in the public,commercial,or not-for-profit sectors.
Authors’ contributions
BB,HP,RK,VT and AM developed the theoretical formalism,performed the analytic calculations and performed the numerical simulations.Both BB and HP contributed to the final version of the manuscript.SNH and BS supervised the project.
Publisher’s note
The Publisher of theJournalremains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
 Asian Pacific Journal of Tropical Medicine2024年3期
Asian Pacific Journal of Tropical Medicine2024年3期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Advances in Zika virus vaccines and therapeutics: A systematic review
- Epidemic management in a measles outbreak in 2023,the return of vaccinepreventable diseases: A single center,retrospective observational study
- Prevalence and risk factors associated with long COVID symptoms in children and adolescents in a southern province of Vietnam
- Characteristics of hospitalized patients with confirmed COVID-19 and their hospital management
