A case of thalamic hemorrhage-induced diaschisis☆
Gang Yao , Yuhong Man Xijing Mao Tingmin Yu
1Department of Neurology, Second Hospital, Jilin University, Changchun 130041, Jilin Province, China
2Department of Neurology, First Hospital, Jilin University, Changchun 130021, Jilin Province, China
INTRODUCTION
Diaschisis refers to a disturbance(inhibition or facilitation) of function in an area remote from the site of a primary brain lesion[1]. Positron emission tomography and single photon emission computed tomography have verified that regional cerebral blood flow and metabolism are clearly decreased in the infarct region[2-4].
Transient excessive perfusion appears in the ischemic penumbra, and diaschisis occurs in an area remote from the lesion site,showing decreased regional cerebral blood flow and metabolism[2-4]. If the above-mentioned phenomenon appears in the contralateral cerebellum, it is called crossed cerebellar diaschisis[5-6]. Mirror diaschisis refers to a decrease in oxygen metabolism and blood flow in the “mirror image area” to the infarct regions in the contralateral hemisphere[7]. Some clinical symptoms and physical signs cannot be explained by primary lesions in stroke patients, which may be associated with diaschisis[8-11]. This study reports on one case of thalamic hemorrhage-induced diaschisis.
CASE INTRODUCTION
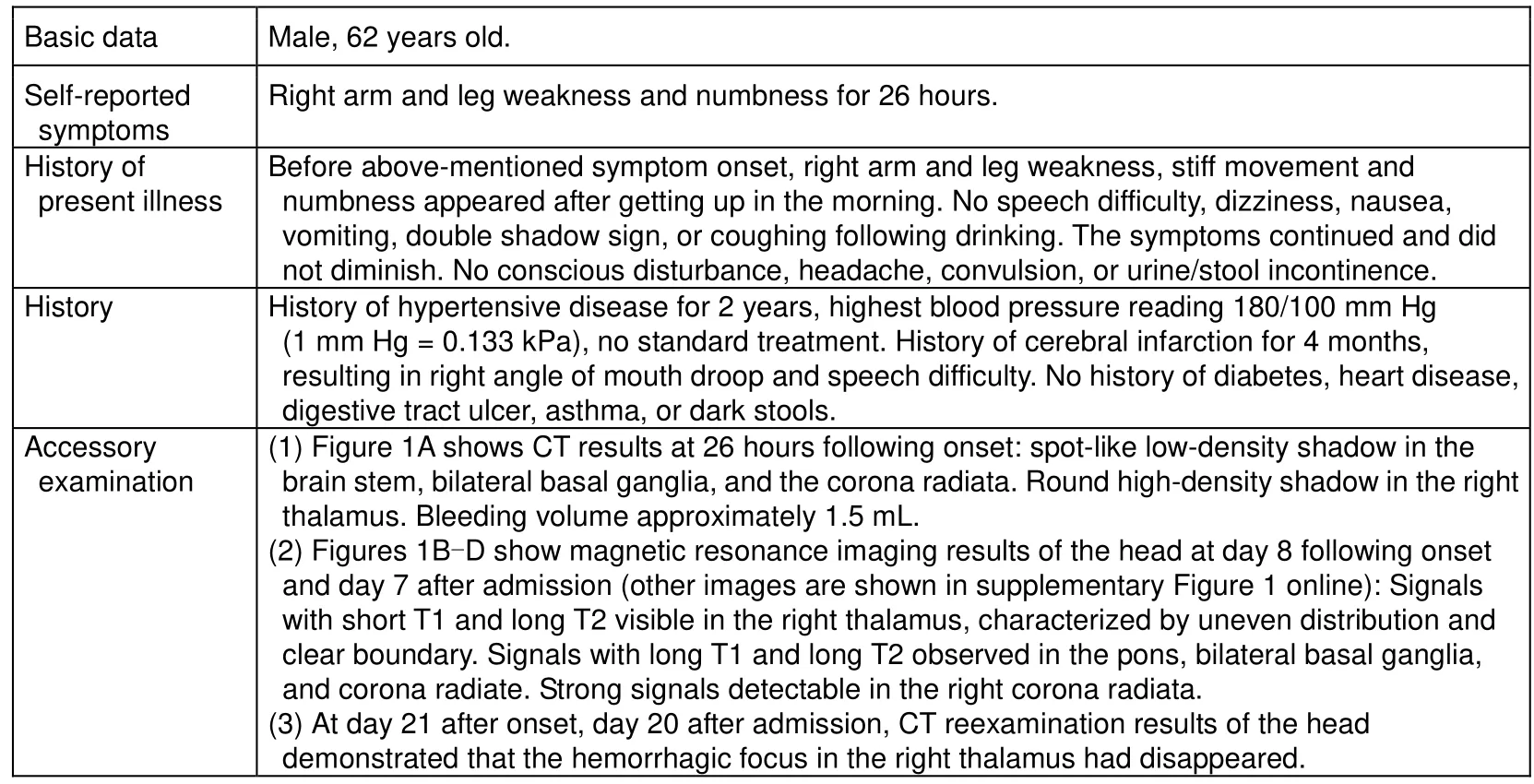
Basic data Male, 62 years old.Self-reported symptoms History of present illness Right arm and leg weakness and numbness for 26 hours.Before above-mentioned symptom onset, right arm and leg weakness, stiff movement and numbness appeared after getting up in the morning. No speech difficulty, dizziness, nausea,vomiting, double shadow sign, or coughing following drinking. The symptoms continued and did not diminish. No conscious disturbance, headache, convulsion, or urine/stool incontinence.History History of hypertensive disease for 2 years, highest blood pressure reading 180/100 mm Hg(1 mm Hg = 0.133 kPa), no standard treatment. History of cerebral infarction for 4 months,resulting in right angle of mouth droop and speech difficulty. No history of diabetes, heart disease,digestive tract ulcer, asthma, or dark stools.Accessory examination(1) Figure 1A shows CT results at 26 hours following onset: spot-like low-density shadow in the brain stem, bilateral basal ganglia, and the corona radiata. Round high-density shadow in the right thalamus. Bleeding volume approximately 1.5 mL.(2) Figures 1B-D show magnetic resonance imaging results of the head at day 8 following onset and day 7 after admission (other images are shown in supplementary Figure 1 online): Signals with short T1 and long T2 visible in the right thalamus, characterized by uneven distribution and clear boundary. Signals with long T1 and long T2 observed in the pons, bilateral basal ganglia,and corona radiate. Strong signals detectable in the right corona radiata.(3) At day 21 after onset, day 20 after admission, CT reexamination results of the head demonstrated that the hemorrhagic focus in the right thalamus had disappeared.
(4) Blood fat: total cholesterol = 6.57 mmol/L. No abnormalities detected in routine blood and urine tests, liver and kidney functions, blood glucose, or myocardial enzyme. No abnormal results in electrocardiography.Body examination after admission Disease evolution Blood pressure 160/100 mm Hg. No abnormities of the heart, lung, and abdomen. Patient conscious, but slight dysarthria and central facial palsy in right side; muscle strength grade 5 in right limbs. Negative pathologic reflex detected, but no local signs observed.(1) At day 2 following admission, body examination showed grip strength of left hand weaker than right hand. Flexibility of left hand fingers decreased. However, patient felt poorer flexibility of right extremities compared with left extremities, and right extremities were numb.(2) At day 5 after admission, muscle strength of right extremities recovered to normal, but the patient still felt flexibility of right extremities poorer than left.(3) At day 8 after admission, grip strength of left hand recovered to normal.(4) At day 12 after admission, the right extremity numbness disappeared.(5) At day 24 after admission, the patient was discharged. The patient still felt that flexibility of the right extremities was poorer than the left side. Body examination: blood pressure 140/80 mm Hg;consciousness; slight dysarthria; central facial palsy in the right side.
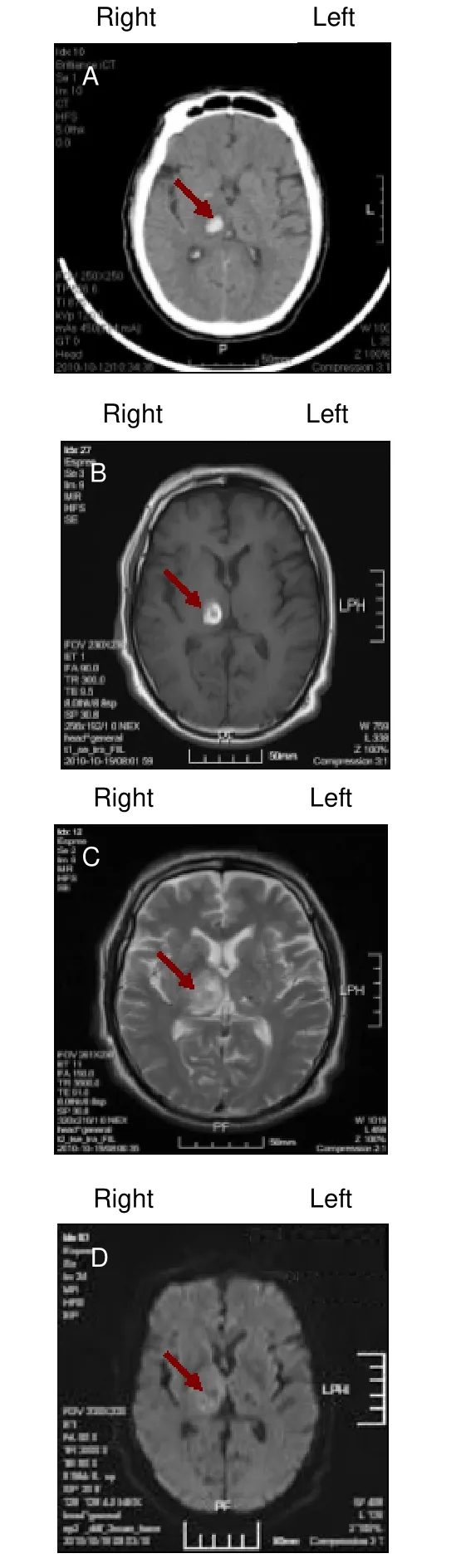
Figure 1 Results of the imaging examination of the cerebral hemorrhage focus. (A) Computer tomography of the head at 26 hours after onset; (B) MRI (T1) of the head at 8 hours after onset; (C) MRI (T2) of the head at 8 hours after onset; (D) MRI (diffusion weighted imaging) of the head at 8 hours after onset. Arrows show the cerebral hemorrhage focus.
DIFFERENTIAL DIAGNOSIS
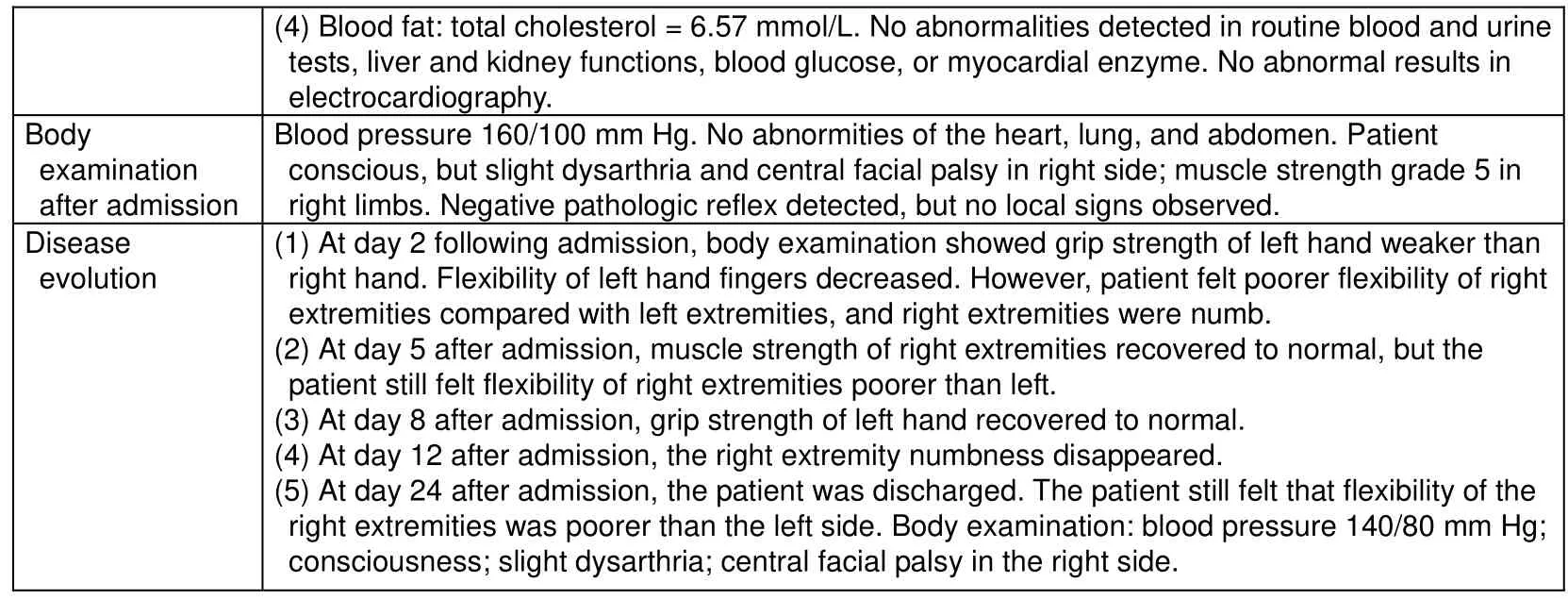
The prominent symptoms of the patient were right arm and leg numbness. At 26 hours following onset, CT of the head exhibited a spot-like low-density shadow in the left thalamus. Results of the MRI of the head demonstrated lacunar infarcts in the left thalamus 4 months prior. Thus,right arm and leg numbness was not associated with lacunar infarcts in the left thalamus (Figures 2A-C).
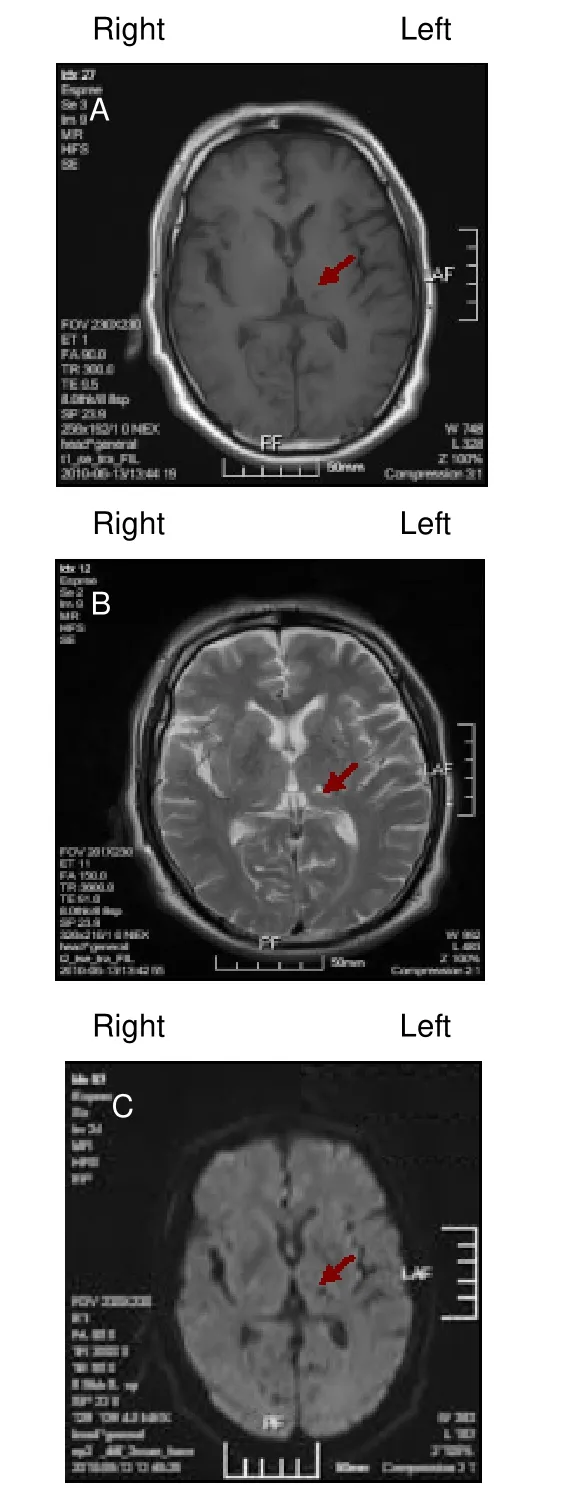
Figure 2 MRI results in a patient with old lacunar infarcts in the left thalamus. (A) T1; (B) T2; (C) diffusion weighted imaging. Arrows show the hemorrhagic focus.
Precise results of MRI are displayed in supplementary Figure 1 online.
At 26 hours following onset, CT of the head did not show the focus that led to the right arm and leg numbness or weakness. To further identify infarct focus in the left hemisphere, the patient received MRI of the head at day 8 following onset (Figures 1B–D). Moreover, the focus that led to right arm and leg numbness or weakness was not detectable.
DISCUSSION ON TREATMENT
After admission, the patient was diagnosed as having thalamic hemorrhage, 3-level hypertension (extremely high risk group), and hyperlipidemia. In accordance with the Administrative Regulations on Medical Institution[12],formulated by the State Council of the People’s Republic of China, the patient was informed of the therapeutic regimen and risk, and signed an informed consent. The patient was administered mannitol to relieve cerebral edema, edaravone to scavenge free radicals, sodium cytidine triphosphate to nourish nerves,enalapril to adjust blood pressure, and probucol to regulate blood fat. The patient refused to use statins,which had previously induced stomach discomfort.
Blood-fat abnormality of the patient only presented with a slightly high level of total cholesterol, and probucol was prescribed.
CONCLUSION
This particular patient had a history of hypertensive disease and a history of ischemic stroke, and was defined with an acute onset of symptoms, showing right arm and leg weakness and numbness. Following admission, body examination showed slight dysarthria and central facial palsy on the right side; muscle strength was grade 5 in the right limbs. Slight dysarthria and central facial palsy on the right side were the result of previous cerebral infarction. At day 2 following admission, body examination showed that the grip strength of the left hand was weaker compared with the right hand. At 26 hours following onset, the CT results displayed in Figure 1A show right thalamic hemorrhage,and lacunar infarction in the brain stem, left thalamus,bilateral basal ganglia, and corona radiata. It is difficult to explain the right arm and leg weakness and numbness with right thalamic hemorrhage. Therefore,the right arm and leg weakness and numbness may be associated with diaschisis. The precise mechanism may be mirror diaschisis. That is, the right thalamic hemorrhage caused decreased oxygen metabolism and blood flow in the “mirror image area” to the infarct regions in the contralateral hemisphere. Unfortunately,the patient could not be persuaded to undergo functional MRI or brain perfusion imaging.
The mechanism of diaschisis remains unclear. Present studies have verified that diaschisis is probably associated with decreased blood flow, effects of neurotoxic substances on distal regions, inhibition of conduction pathways, degenerative changes in axons,neurotrophic factor problems, neurotransmitter abnormalities, neuroendocrine disturbance, neuronal apoptosis, and disruption of neuronal repair[13-16].
Diaschisis is an important pathophysiological phenomenon of stroke. Clinical symptoms that appear unrelated to the focus probably represent the occurrence of diaschisis. Basic and clinical studies of diaschisis in stroke will also further reveal cerebral function.
Author contributions:Gang Yao was the physician in charge of the patient enrolled in this report, participated in case analysis, and manuscript writing. Yuhong Man and Xijing Mao provided case data and participated in the case analysis.Tingmin Yu was responsible for the case analysis and manuscript authorization, and for the therapeutic regimen.
Conflicts of interest:None declared.
Supplementary information:Supplementary data associated with this article can be found, in the online version, by visiting www.nrronline.org, and entering Vol. 6, No. 23, 2011 after selecting the “NRR Current Issue” button on the page.
[1]Feeney DM, Baron JC. Diaschisis. Stroke.1986;17(5):817-830.
[2]Hu WM, Wang WZ. Q&A 900 for Attending Neurolgist. Beijing:Peking Union Medical College Press. 2007.
[3]Lin DD, Kleinman JT, Wityk RJ, et al. Crossed cerebellar diaschisis in acute stroke detected by dynamic susceptibility contrast MR perfusion imaging. AJNR Am J Neuroradiol.2009;30(4):710-715.
[4]Brodtmann A, Puce A, Darby D, et al. fMRI demonstrates diaschisis in the extrastriate visual cortex. Stroke. 2007;38(8):2360-2363.
[5]Kishi M, Sakakibara R, Nagao T, et al. Isolated hemiataxia and cerebellar diaschisis after a small dorsolateral medullary infarct.Case Rep Neurol. 2009;1(1):41-46.
[6]Garg G, Tripathi M, D'Souza MM, et al. Crossed cerebellar diaschisis demonstrated by(18)F-FDG-PET/CT. Hell J Nucl Med.2009;12(2):171-172.
[7]Baron JC, Levasseur M, Mazoyer B, et al. Thalamocortical diaschisis: positron emission tomography in humans. J Neurol Neurosurg Psychiatry. 1992;55(10): 935-942.
[8]Paradowski B, Pawlik B. Diaschisis phenomenon in different neurological diseases. Wiad Lek. 2005;58(11-12):675-677.
[9]Cianfoni A, Luigeti M, Bradshaw ML, et al. MRI findings of crossed cerebellar diaschisis in a case of Rasmussen's encephalitis. J Neurol. 2010;257(10):1748-1750.
[10]Samaniego EA, Stuckert E, Fischbein N, et al. Crossed cerebellar diaschisis in status epilepticus. Neurocrit Care. 2010;12(1):88-90.
[11]Ribacoba R, Menéndez M, Salas-Puig J. Refractory epilepsy and crossed cerebellar diaschisis. Neurologia. 2009;24(3):211-213.
[12]State Council of the People's Republic of China. Administrative Regulations on Medical Institution. 1994-09-01.
[13]Kajimoto K, Oku N, Kimura Y, et al. Crossed cerebellar diaschisis:a positron emission tomography study with L-[methyl-11C]methionine and 2-deoxy-2-[18F]fluoro-D-glucose. Ann Nucl Med.2007;21(2):109-113.
[14]Xiong L, Zeng JS. Advance in research on secondary damage remote from middle cerebral artery infarction. Guowai Yixue:Neikexue Fence. 2005;13(11):835-838.
[15]Wang C, Xiong YB, Liu CX. The mehanism of secondary damage in remote regions after cerebral hemorrhage. Yixue Xinxi(Shoushuxue Fence). 2009;22(1):56-58.
[16]Stenset V, Grambaite R, Reinvang I, et al. Diaschisis after thalamic stroke: a comparison of metabolic and structural changes in a patient with amnesic syndrome. Acta Neurol Scand Suppl. 2007;187:68-71.
 中國(guó)神經(jīng)再生研究(英文版)2011年23期
中國(guó)神經(jīng)再生研究(英文版)2011年23期
- 中國(guó)神經(jīng)再生研究(英文版)的其它文章
- NIH funding for disease categories related to neurodegenerative diseases
- Occlusion of the middle cerebral artery Guidance by screen imaging using an EDA-H portable medium-soft electronic endoscope☆
- Propofol regulates Ca2+, Mg2+, Cu2+ and Zn2+ balance in the spinal cord after ischemia/reperfusion injury***★
- Using Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry to analyze differentially expressed brain polypeptides in scrapie strain 22L-infected BALB/c mice***☆
- Optimal velocity encoding during measurement of cerebral blood flow volume using phase-contrast magnetic resonance angiography*☆
- Evidence-based treatment for acute spinal cord injury☆
