Maternal outcome in multiple versus singleton pregnancies in Northern Tanzania: A registry-based case control study
Enid Simon Chiwanga, Gileard Massenga,2, Pendo Mlay,2, Joseph Obure,2,3, Michael Johnson Mahande
1Department of Obstetrics & Gynecology, Kilimanjaro Christian Medical Centre(KCMC)/Kilimanjaro Christian Medical Collage (KCM College), Moshi, Tanzania
2Department of Community Health, Kilimanjaro Christian Medical UniversityCollege, Moshi, Tanzania
3Walter Reed Southern Highlands HIV/AIDS Care Program-Mbeya, Tanzania
Maternal outcome in multiple versus singleton pregnancies in Northern Tanzania: A registry-based case control study
Enid Simon Chiwanga1, Gileard Massenga1,2, Pendo Mlay1,2, Joseph Obure1,2,3, Michael Johnson Mahande2*
1Department of Obstetrics & Gynecology, Kilimanjaro Christian Medical Centre(KCMC)/Kilimanjaro Christian Medical Collage (KCM College), Moshi, Tanzania
2Department of Community Health, Kilimanjaro Christian Medical UniversityCollege, Moshi, Tanzania
3Walter Reed Southern Highlands HIV/AIDS Care Program-Mbeya, Tanzania
ARTICLE INFO
Article history:
Received 6 November 2013
Received in revised form 25 November 2013
Accepted 25 November 2013
Available online 20 January 2013
Maternal outcome,
Objective: To compare maternal outcome of multiple versus singleton pregnancies at a tertiary hospital in Tanzania. Methods: A case control study was designed using maternally linked data from Kilimanjaro Christian Medical Centre (KCMC) medical birth registry for the period of 2000-2010. A total of 822 multiple gestations (cases) were matched with 822 singletons (controls) with respect to maternal age at delivery and parity. The odds ratio (ORs) with 95% confidence intervals (CIs) for adverse maternal outcome between singleton and multiple gestations were computed in a multivariable logistic regression model. Results: Of the 33 997 births, there were 822 (2.1%) multiples. Compared with singletons, women with multiple gestations had increased risk for preeclampsia (OR 2.6; 95% CI: 1.7-3.9), preterm labour (OR 5.6; 95% CI: 4.2-7.4), antepartum haemorrhage (OR 1.6; 95% CI: 1.1-2.3), anaemia (OR 2.0; 95% CI: 1.6-2.6) and caesarean section (OR 1.5; 95% CI: 1.4-1.7). In addition, there were six maternal deaths among women with multiple gestations, of which all were attributed to postpartum haemorrhage. This accounted for a case fatality rate of 15.8%. Conclusions: Multiple gestations are associated with adverse maternal outcomes. Close follow-up and timely interventions may help to prevent poor outcomes related to multiple gestations. These findings suggest the needs for clinicians to counsel women with multiple gestations during prenatal care regarding the potential risks.
1. Introduction
Multiple gestations or multiple pregnancies occur when two or more foetuses are conceived at the same time in the same woman, it can either be a monozygotic or dizygotic pregnancy [1]. Multiple gestations are associated with increased fetal-maternal complications [2-4].
Although the rates of multiple pregnancies have shown to decline in Europe over the last decades, these rates are still higher compared to those reported in developing countries. For example, in Europe, incidence of multiple pregnancies rates was 21.7% in 2008 compared with 22.3% in 2007, 20.8% in 2006 and 21.8% in 2005 respectively [5-7]. Recent studies in Nigeria reported a twinning rate ranging from 1.4%-4.7% [8-11]. The higher multiple pregnancy rate in Europe is attributed to the increased use of assisted reproductive techniques as well as the use of ovulation stimulation agents [12, 13].
The risk factors for multiple gestation births have been well documented [14, 15]. These include family history of twins, heredity, advanced age, serum oestradiol concentration, race, and use of fertility treatment.
Furthermore, women with multiple gestations are at increased risk of preeclampsia, preterm labour, delivery of low birth weight infant, antepartum or postpartumhaemorrhage, caesarean section delivery, congenital anomalies, intrauterine growth retardation, maternal and perinatal death as compared to women with singleton gestations [16-19]. In addition, multiple gestations are associated with increased cost to families and health care system [20-23]. All these factors are the reasons why multiple pregnancies remain a major public health problem as compared to singleton pregnancies, particularly in sub Saharan Africa, given the high maternal mortality rate in the region.
There are limited information about maternal-fetal outcome and complications of twins’ pregnancy in Tanzania. Previous hospital-based studies in Tanzania reported variations in prevalence of multiple gestations, ranging from 15-29 per 1 000 births [24-26]. These studies did not explore the differences in maternal-fetal outcomes and complications between multiple and singleton pregnancies. Therefore this study provides relevant clinical and public health information that may help to inform policy and clinicians on how to manage multiple pregnancies in the country. In addition, findings from this study may help as basis for further intervention research studies that could help to improve maternal and foetal outcomes.
The objective of this study was to compare maternal outcomes between mothers with singleton and those with multiple gestations.
2. Materials and methods
2.1. Study setting
Kilimanjaro Christian Medical Centre (KCMC) is located in Moshi municipal, Kilimanjaro Tanzania. It’s one among the four tertiary and zonal referral hospitals in Tanzania. The centre provides delivery services to pregnant women from the nearby communities as well as referral cases from other regions. It has an average of 3 000 deliveries per year.
The KCMC medical birth registry was established in 1999 as collaborative project between KCMC and the Medical Birth Registry in Norway, and it has been in operation since 2 000. Since then, information for all deliveries that occur at the department of Obstetrics and Gynaecology are prospectively collected and entered in a computerized database system at the medical birth registry.
2.2. Study design
A case control study was designed using KCMC medical birth registry maternally linked data from 2000 to 2010. KCMC medical birth registry provide linked data, with exact linkage of birth records for parents and their siblings through the mother unique identification number assigned to each woman who deliver for the first time at KCMC. This number is constant for subsequent births that occur at KCMC. A total of 33 997 births were recorded at the medical birth registry from year 2000-2010, of these 822 were multiple births. Mothers were linked with their sibling records using a unique mother’s identification hospital number.
2.3. Selection of cases and controls
This study included 822 multiple gestations (cases) and 822 singletons (controls) who delivered at 28 weeks of gestation or more with complete study information as per birth registry database. Cases and control were matched with the 1:1 ratio based on maternal age at delivery and parity. Cases and controls were frequency matched for age group (<18 years, 18-25, 26-35, >35) and parity group (0, 1, 2, ≥3) to gain precision and facilitate control of confounding. Frequency matching was preferred over individual matching for logistical reasons, where proportions of controls were matched with same proportion of cases with respect to the matched variables to enhance similar distribution. Furthermore, women with singleton or multiple gestations completing 28 weeks of gestation with or without medical and obstetric complications were included. We excluded births with incomplete information and those with duplicate maternal identification number.
2.4. Data collection
Trained nurse midwives used a standardized questionnaire to conduct interview on daily basis for each woman within 24 hours after delivery or later in case a mother experienced some complications. Additional information was obtained from maternal antenatal cards for verification of some prenatal information. Verbal consent was sought from each individual woman prior to the interview after a mother being explained objectives and benefits of the medical birth registry project. The details of information that are collected have been described elsewhere [27]. In summary, information collected includes maternal and paternal sociodemographic characteristics, prepregnancy and pregnancy medical conditions, postpartum conditions and pregnancy outcomes. Finally, all data collected are immediately entered into a computerized database system at the birth registry.
Our main outcomes of interest were maternal outcomes including preeclampsia, preterm labour, premature rupture of membranes, antepartum (APH) and postpartum haemorrhage (PPH) , anaemia and caesarean section delivery.
2.5. Statistical analysis
Data were analyzed using Statistical Package for Social Science (SPSS) 17.0 (SPSS, Inc., Chicago, Illinois, USA). The student samples t-test was used to compare means for continuous outcome between the study groups. The chi square test (χ2) was used for comparison of proportions for categorical variables. The odds ratio (ORs) with 95% confidence intervals (CIs) for adverse maternal outcome between singleton and multiple gestations were computed in a multivariable logistic regression model. The independent variables included in the multivariable logistic regression model were matching variables (age group and parity) and other maternal characteristics such as area of residence, maternal education, and mother’s tribe. We also adjusted for preeclampsia on preterm delivery. A P value of less than 5% was considered statistically significant.
2.6. Ethical consideration
This study was approved by the Kilimanjaro Christian Medical University College(KCMU-College) Research Ethics Committee prior its commencement.
3. Results
3.1. Demographic characteristics of the study participants
There were 39 977 deliveries registered from 2000 to 2010. Of these 822 (2.1%) were multiple pregnancies, resulting to twinning rate of 21 per 1 000 births.
The sociodemographic characteristics of participants are depicted in Table 1. The mean age (SD) between women with multiple and singleton gestations was 29 (5.7) years. More than half (58.9%) of the participants were aged between 26-35 years. The mean gestational age at delivery for women with multiple gestations was lower compared with that of singletons (36.0 ±3.4 vs. 39.0±3.6) weeks, respectively. Women with multiple gestations were significantly more likely to report living in rural areas as compared to their singleton counterparts (55.8% vs. 44.9%, P<0.001). There was no significant difference between the two groups with regards to attendance to antenatal care (P=0.53).
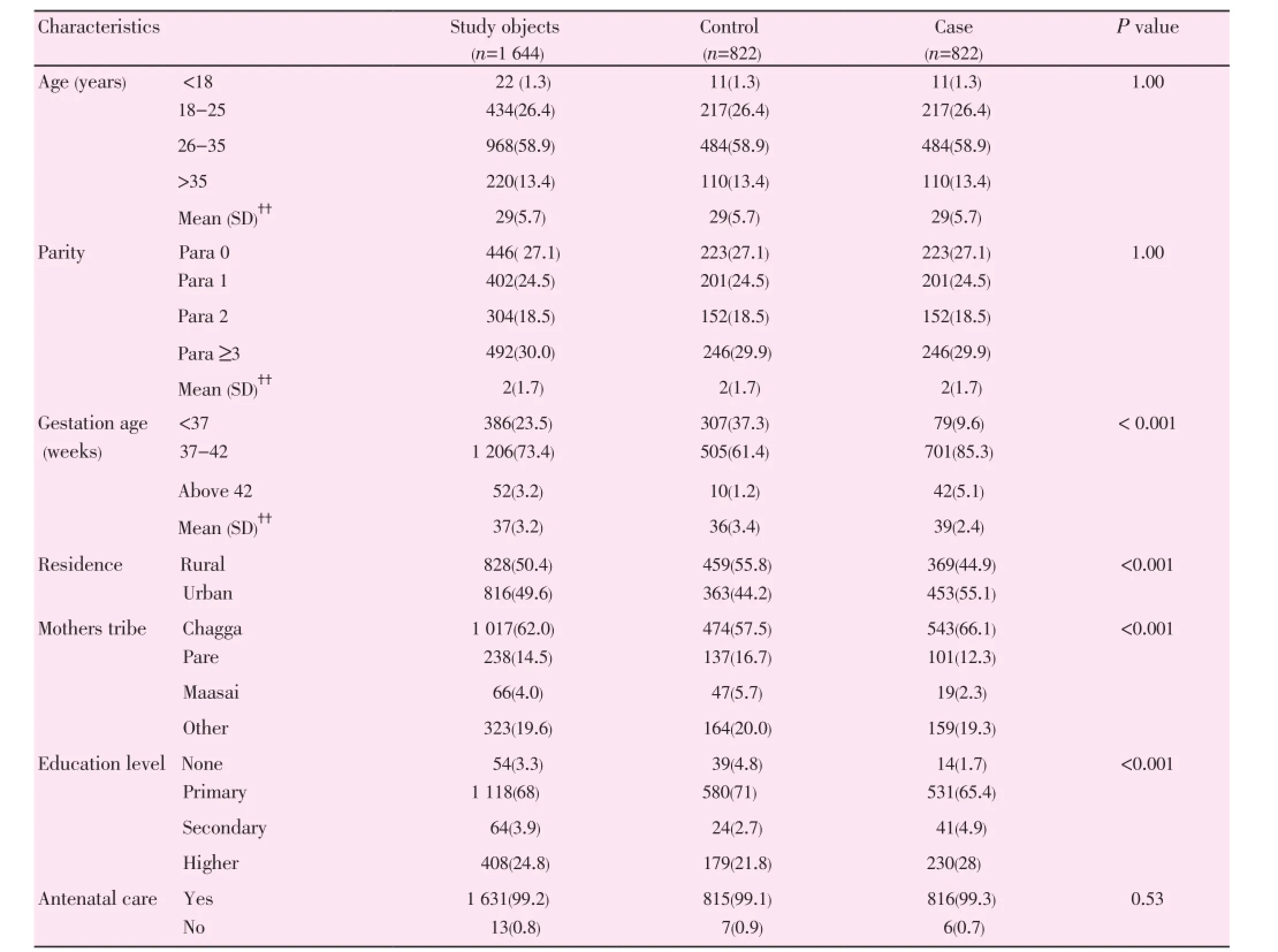
Table 1Comparison of maternal demographic characteristics between cases and controls.
3.2. Maternal outcomes among cases and controls
Table 2 summaries results from a multivariate regression analysis. Overall, women with multiple gestations had significantly higher rates of preterm birth as compared to women with singletons gestations (37.3% vs. 9.6%; P<0.001). The corresponding odds ratio was (5.6; 95% CI: 4.2-7.4). Likewise, women with multiple gestations had a 2.6-fold (95% CI: 1.7-3.9) increased risk of preeclampsia as compared to controls. Furthermore, women with multifetal gestations had increased risk for anaemia (OR 2.0; 95% CI: 1.6-2.6), antepartum haemorrhage (OR 1.6; 95% CI: 1.1-2.3), and caesarean section delivery (OR 1.5; 95% CI: 1.4-1.7) compared with their singleton counterparts. It is worth noting that, the risks for postpartum haemorrhage and premature rupture of membranes were higher for women with multiple gestations as compared to singleton mothers (2.2, 95% CI: 0.8-5.8; and 1.1, 95% CI: 0.8-1.5, respectively). In addition, postpartum haemorrhage was associated with six maternal deaths among multiple gestations. This accounted for a case fatality rate of 15.8% (6/38 × 100).
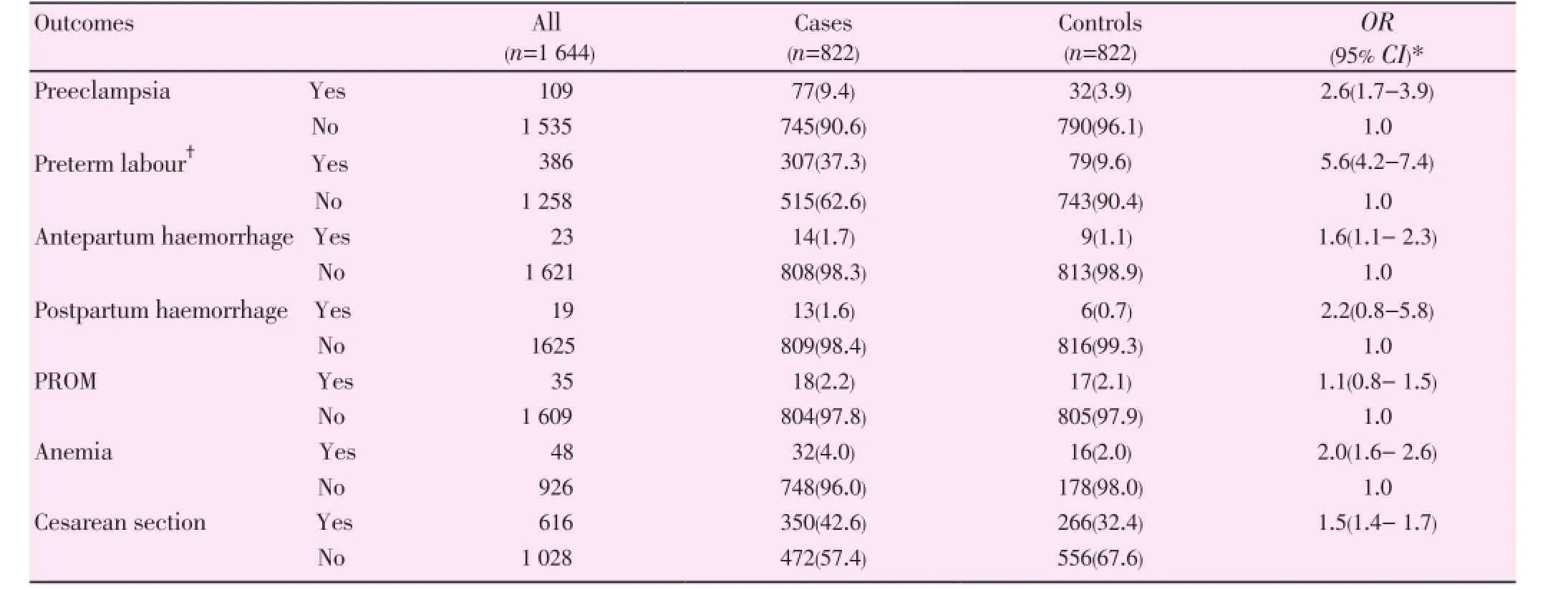
Table 2Multiple logistic regression with back ward elimination of adverse maternal outcomes between cases and controls.
*Adjusted for area of residence, maternal education, tribe, maternal age at delivery and parity,?Adjusted for preeclampsia and all above
4. Discussion
In this study, we compared maternal outcomes between singleton and multiple gestations. Our study confirmed that women with multiple gestations have increased risk of preeclampsia, preterm delivery, anaemia, caesarean section delivery, antepartum and postpartum haemorrhage as compared to women with singleton gestations. In addition, the case fatality rate among women with PPH was significantly higher in multiple gestation pregnancy compared to singleton pregnancy.
In the present study, the twinning rate was 21 per 1 000 births which was consistent with previous findings in Tanzania and Kenya using hospital data [24-26,28]. But it was lower compared to that reported by Nigerian investigators [8, 9, 11,29-34] who found the twinning rates of 26.0-46.5 per 1 000 births, and others in developed countries [6, 7, 35, 36]. However, the twinning rate observed in our study was slightly higher than 18 per 1 000 births that was recently reported from a community-based study in Guinea-Bissau [37]. The variations in twinning rate may be explained by the differences in prevalence of the risk factors for twinning between the studied populations including family history of multiple pregnancies and sample size. Furthermore, the higher twinning rate reported by Nigerian investigators could be due to a higher referral rate from other hospitals which couldn’t handle complications related to multiple pregnancies.
In this study, women with multiple gestations had a 6-fold increased risk of experiencing preterm delivery as compared to their singleton counterparts. Our result was in agreement with previous studies [3, 16, 17]. Furthermore, the corresponding preterm delivery rate of 37.3% in multiple gestations observed in our study was also demonstrated by previous studies in the region [34, 36, 38, 39]. However, otherinvestigators [10, 40] showed higher rates of preterm delivery in their studies (74% and 84%, respectively) . The higher rate of preterm delivery in the previous studies could be explained by other complications associated with multiple gestations such as premature rupture of membranes or preeclampsia, which requires early intervention for termination of the pregnancy.
We observed a 2.6-fold increased risk of developing preeclampsia in women with multiple gestations. Several studies [8, 11, 31, 33, 34] also reported similar finding. However, the corresponding absolute risk of preeclampsia of 9.4% in our study was lower than that reported by the previous investigators [38, 41] who found the preeclampsia rate of 28% and 31% respectively The reason for higher rates of preeclampsia in the previous studies might be explained by high prevalence of preeclampsia associated with other reason other than multiple pregnancy or a high pre-existing maternal medical conditions.
In the present study, caesarean section was observed in (43%) of the cases as compared to (32.4%) in the control group. This fiding was consistent with previous studies in the region [8, 39]. The caesarean rate observed in our study falls within a range of 42%-51.2% that was reported at teaching hospital in Nigeria [33, 42]. But it was above the range of 7.3%-31.7% that was reported at a tertiary centers in Nigeria [30, 33, 34] and lower than 53.3% in the USA by Qazi [36]. The relatively higher caesarean section rate in our study and others could be explained by the coassociation of multiple pregnancy and other poor obstetric outcomes such as preeclampsia/eclampsia, fetal distress, malpresentation and premature rupture of membranes which necessitate caesarean section delivery to reduce severe maternal and fetal complications [43].
In the present study, mothers with multiple gestations had a 2-fold increased risk of maternal anemia compared with singleton gestations mothers. Our finding was in line with the previous reports [10, 36, 38]. However, it is important to point out that the rate of anemia was only 4% in our study which was lower as compared to the previous reports. The reason for lower rate of anemia in the present study could be attributed to the increased uptake of iron and folic acid supplements during antenatal care services.
Olusanya [8] reported a 1.2-fold increased risk of antepartum haemorrhage among Nigerian women who delivered twins compared with those who had singleton delivery. This was slightly lower compared to corresponding risk observed in the present study and others [33, 38]. The difference in risk of antepartum haemorrhage between studies could be explained by the differences in the risk factors for antepartum haemorrhage between the studied populations.
In the present study, the PPH rate was 1.6% higher in the multiple gestations group compared to singletons. Consistent with this study, Musili et al in Kenya [28] also found a significant increase in postpartum haemorrhage in multiple gestations compared to single tone gestation. However, the rate of PPH in our study was lower than 12.5% and 16% that was reported in the previous [10, 38]. The lower PPH rate in our study could be attributed to increased access to quality emergency obstetric care, in particular the use of active management of the third stage of labour.
Furthermore, our study revealed 6 deaths in association to post partum hemerrhage in multiple pregnancy compared to none in singleton births. This constitutes to case fatality rate of 15.8%. The difference could be related to the presence of other pre-existing medical conditions in multiple gestations group.
Previous studies in Nigeria reported a higher incidence of premature rupture of membrane in a range of 28.0%-84.4% in women with multiple gestations than in singleton gestations [10, 38]. Likewise, a study in the USA by Qazi [36] reported the rate of 26% in women with multiple gestations compared with singleton gestations. In contrast, the premature rupture of membranes rate in our study was lower than the previous studies, but it was similar to that reported by Akaba et al [34]. The higher rate of premature rupture of membranes in the American study could be related to increased number of fetus in multi-fetal gestations due to increased use of ovulation inductions and assisted reproductive technology, while in Nigeria it could be related to the increase in other risk for premature rupture of membranes such as infection with group B beta hemolytic streptococcal.
Our findings suggests that reinforcing referral to specialized facilities that may provide advance obstetric care may be of importance for women with multiple gestations in order to improve pregnancy outcomes, while series of ultrasonographic cervical length assessment can help identify multiple pregnancies at risk for preterm labor hence providing opportunity for early interventions. The strengths of our study include access to a large data set from a cohort of women with multiple gestations. This is the first large study in Tanzania and probably in East African region in particular to utilize a prospectively collected data on multiple pregnancies. The large sample size increases the power to detect the association between exposure and outcome studied. Our results therefore can be generalized to other women who deliver in the similar settings in Tanzania. The use of prospectively collected data minimizes recall bias which is common problem in many retrospective studies and tradition case control studies. The identified maternal outcome associated with multiple gestations agreeswith several studies in the region that were conducted in the similar settings. The rich database allowed for adjustment for multiple clinical and socioeconomic variables that may have confounded the study results.
Our study also has some limitations, which need to be considered while interpreting our results. First, this was the hospital-based study, conducted at a referral hospital and hence there could be a chance for selection bias, as most of the complicated pregnancy cases are attended in this facility. Women who delivered outside the KCMC might have different characteristics to those who delivered at KCMC. If that is true, our risk estimates (ORs) could have been overestimated. This could compromise generalizability of our findings to other women in the general population.
Secondly, this study estimated gestation age based on the woman last normal menstrual period. This may results in the misclassification bias of the preterm births. However, if this problem has happened, then its effect could lead to nondifferential misclassification bias.
Third, unfortunately we were not able to adjust for potential confounder for obstetric factors in the previous pregnancy, family history as a possible confounder for twinning, paternity between pregnancies and history of preeclampsia or severe preterm birth as risk factors for preeclampsia and previous preterm birth which may influence the risk of preterm in subsequent pregnancy. The effect of these variables in our results remains unclear.
Our study indicates that multiple gestations are associated with increased risks of preterm delivery, preeclampsia, anaemia, caesarean section delivery, antepartum and postpartum haemorrhage. This calls for the increased access to early diagnosis by providing at least one obstetric ultrasound at mid second trimester to confirm the diagnosis of multiple pregnancies and provide referrals to a more specialized care. Our finding also underscores the need for prenatal counselling on potential complications and what to do when they occur. Further population-based study is required to confirm our findings and explore the role of recurrence of twinning and family history of twinning.
Conflict of interest statement
We declare that we have no conflict of interest .
Acknowledgements
We thank the Norwegian Council for Higher education program and Development Research (NUFU) for supporting the birth registry at KCMC. We also thank for the birth registry staff for their participation in data collection. More important, we appreciate for women who delivered at KCMC to provide information which enabled this study to be done.
[1] Wimalasundera R, Fisk NM. In-vitro fertilisation and risk of multiple pregnancy. The Lancet 2002; 360(9330): 414.
[2] Prapas N, Kalogiannidis I, Prapas I, Xiromeritis P, Karagiannidis A, Makedos G. Twin gestation in older women: antepartum, intrapartum complications, and perinatal outcomes. Arch Gynecol Obstet 2006; 273(5): 293-297.
[3] Mazhar S.B. PA, Mahmud G. Maternal and perinatal complications in multiple versus singleton pregnancies: A prospective two years study. J Pak Med Assoc 2002; 52(4): 143-147.
[4] Wen SW, Demissie K, Yang Q, Walker MC. Maternal morbidity and obstetric complications in triplet pregnancies and quadruplet and higher- order multiple pregnancies. Am J Obstet Gynecol 2004; 191(1): 254-258.
[5] Nyboe Andersen A, Goossens V, Bhattacharya S, Ferraretti AP, Kupka MS, de Mouzon J, et al. The European IVF-monitoring consortium ftESoHR, embryology: Assisted reproductive technology and intrauterine inseminations in Europe, 2005: results generated from European registers by ESHRE. Hum Reprod 2009; 24(6): 1267.
[6] de Mouzon J, Goossens V, Bhattacharya S, Castilla JA, Ferraretti AP, Korsak V, et al. Assisted reproductive technology in Europe, 2007: results generated from European registers by ESHRE. Hum Reprod 2012; 27(9): 2571-2584.
[7] de Mouzon J, Goossens V, Bhattacharya S, Castilla JA, Ferraretti AP, Korsak V, et al. Assisted reproductive technology in Europe,2006: results generated from European registers by ESHRE. Hum Reprod 2010; 25(8): 1851-1862.
[8] Olusanya BO. Perinatal outcomes of multiple births in southwest Nigeria. J Health Popul Nutr 2011; 29(6): 639-647.
[9] Fakeye O. Perinatal factors in twin mortality in Nigeria. Int J Gynaecol Obstet 1986; 24(4): 309-314.
[10] Rizwan N, Abbasi RM, Mughal R. Maternal morbidity and perinatal outcome with twin pregnancy. J Ayub Med Coll Abbottabad 2010; 22(2): 105-107.
[11] Akinboro A, Azeez MA, Bakare AA. Frequency of twinning in southwest Nigeria. Indian J Hum Genet 2008; 14(2): 41-47. .
[12] Botting BJ, Davies IM, Macfarlane AJ. Recent trends in the incidence of multiple births and associated mortality. Arch Dis Child 1987; 62(9): 941-950.
[13] Martin JA Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Kirmeyer S, et al. Births: final data for 2007. Natl Vital Stat Rep 2007; 58(24): 1-85.
[14] Tur R, Barri PN, Coroleu B, Buxaderas R, Martínez F, Balasch J. Risk factors for high-order multiple implantation after ovarian stimulation with gonadotrophins: evidence from a large series of1878 consecutive pregnancies in a single centre. Hum Reprod 2001; 16(10): 2124-2129.
[15] Dickey RP, Taylor SN, Lu PY, Sartor BM, Rye PH, Pyrzak R. Relationship of follicle numbers and estradiol levels to multiple implantation in 3 608 intrauterine insemination cycles. Fertil Steril 2001; 75(1): 69-78.
[16] Shebl O ET, Sir A, Sommergruber M, Tews G. The role of mode of conception in the outcome of twin pregnancies. Minerva Ginecol 2009; 61(2): 141-152.
[17] Garg P, Abdel-Latif ME, Bolisetty S, Bajuk B, Vincent T, Lui K. Perinatal characteristics and outcome of preterm singleton, twin and triplet infants in NSW and the ACT, Australia (1994-2005). Arch Dis Child - Fetal and Neonatal Edition 2010; 95(1): F20-F24.
[18] Helmerhorst FM, Perquin DAM, Donker D, Keirse MJNC. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ 2004; 328(7434): 261.
[19] Ballabh P, Kumari J, AlKouatly HB, Yih M, Arevalo R, Rosenwaks Z, et al. Neonatal outcome of triplet versus twin and singleton pregnancies: a matched case control study. Eur J Obstet Gynaecol Reprod Biol 2003; 107(1): 28-36.
[20] Callahan TL, Hall JE, Ettner SL, Christiansen CL, Greene MF, Crowley WF. The economic impact of multiple-gestation pregnancies and the contribution of assisted-reproduction techniques to their incidence. New Engl J Med 1994; 331(4): 244-249.
[21] De Sutter P, Gerris J, Dhont M. A health-economic decisionanalytic model comparing double with single embryo transfer in IVF/ICSI. Hum Reprod 2002; 17(11): 2891-2896.
[22] Kinzler WL, Ananth CV, Vintzileos AM. Medical and economic effects of twin gestations. J Soc Gynecol Investig 2000; 7(6): 321-327.
[23] Lukassen HGM, Sch?nbeck Y, Adang EMM, Braat DDM, Zielhuis GA, Kremer JAM. Cost analysis of singleton versus twin pregnancies after in vitro fertilization. Fertil Steril 2004; 81(5): 1240-1246.
[24] Van RJ. Multiple pregnancy as a risk factor in rural Tanzania. Trop Geogr Med 1988; 40(3): 196-200.
[25] Adamson H. Low birth weight in relation to maternal age and multiple pregnancies at Muhimbili National Hospital. DMSJ 2006; 14(2): 55.
[26] Peter B. Prevalence of twin deliveries and perinatal outcomes in public hospitals in Dar es Salaam. MMed (Obstetrics and Gynaecology) Dissertation submitted to Muhimbili University of Health and Allied Sciences; 2012.
[27] Mmbaga B, Lie R, Kibiki G, Olomi R, Kvale G, Daltveit A. Transfer of newborns to neonatal care unit: a registry based study in Northern Tanzania. BMC Pregnancy Childbirth 2011; 11(1): 68.
[28] Musili FKJ. Multifoetal pregnancies at a maternity hospital in Nairobi. East Afr Med J 2009; 86(4): 162-165.
[29] Igberase GO, Ebeigbe PN, Bock-Oruma A. Twinning rate in a rural mission tertiary hospital in the Niger delta, Nigeria. J Obstet Gynaecol 2008; 28(6): 586-589.
[30] Onah HE, Ugwu GO. Trends in twinning rate in Enugu, Nigeria. J Obstet Gynaecol 2008; 28(6): 590-592.
[31] Iyiola OA, Oyeyemi FB, Raheem UA, FO M. Frequency of twinning in Kwara State, North-Central Nigeria. The Egyptian J Med Hum Genet 2013; 14: 29-35.
[32] Sunday-Adeoye I, Twomey ED, Egwuatu VE. A 20-year review of twin births at Mater Misericordiae Hospital, Afikpo, South Eastern Nigeria. Niger J Clin Pract 2008; 11(3): 231-234.
[33] Abasiattai AM, Umoiyoho AJ, Utuk NM, Shittu DG. Incidence and mode of delivery of twin pregnancies in Uyo, Nigeria. Niger Med J 2010; 51(4): 170-172.
[34] Akaba GO, Agida TE, Onafowokan O, Offiong RA, Adewole ND. Review of twin pregnancies in a tertiary hospital in Abuja, Niger. Health Popul Nutr 2013; 31(2): 272-277.
[35] Nyboe Andersen A, Goossens V, Bhattacharya S, Ferraretti AP, Kupka MS, de Mouzon J, et al. The European IVF-monitoring Consortium ftESoHR, Embryology: Assisted reproductive technology and intrauterine inseminations in Europe, 2005: results generated from European registers by ESHRE. Hum Reprod 2009; 24(6): 1267-1287.
[36] Qazi G. Obstetric and perinatal outcome of multiple pregnancy. J Coll Physicians Surg Pak 2011; 21(3): 142-145.
[37] Bjerregaard-Andersen M, Lund N, Jepsen F, Camala L, Gomes M, Christensen K, et al. A prospective study of twinning and perinatal mortality in urban Guinea- Bissau. BMC Pregnancy Childbirth 2012; 12(1): 1-12.
[38] Sultana M, Khatun S, Saha AK, Akhter P, Shah AS. Maternal and perinatal outcome of twin pregnancy in a tertiary hospital. Ibrahim Card Med J; 2011;1(2): 35-39.
[39] Mutihir JT, Pam VC. Obstetric outcome of twin pregnancies in Jos, Nigeria. Niger J Clin Pract 2007; 10(1): 15-18.
[40] Hanumaiah I, Shivanand DR , Visweshwaraiah KG, Hoolageri MS. Perinatal outcome of twin pregnancies at a tertiary care centre, south india. Int J Biol Med Res 2013; 4(1): 2683-2685.
[41] Foo JY, Mangos GJ, Brown MA. Characteristics of hypertensive disorders in twin versus singleton pregnancies. Pregnancy Hypertension: An International Journal of Women’s Cardiovascular Health 2013; 3(1): 3-9.
[42] Obiechina NJ, Okolie VE, Eleje GU, Okechukwu ZC, Anemeje OA. Twin versus singleton pregnancies: the incidence, pregnancy complications, and obstetric outcomes in a Nigerian tertiary hospital. Int J Womens Health 2011; 3: 227-230.
[43] Worjoloh A, Manongi R, Oneko O, Hoyo C, Daltveit AK, Westreich D. Trends in cesarean section rates at a large East African referral hospital from 2005-2010. OJOG 2012; 2: 255-261.
ment heading
10.1016/S2305-0500(14)60001-4
*Corresponding author: Michael Johnson Mahande, Department of Community Health, Kilimanjaro Christian Medical University College, Moshi, Tanzania.
E-mail: jmmahande@gmail.com
Multiple gestations
Registry-based study
 Asian Pacific Journal of Reproduction2014年1期
Asian Pacific Journal of Reproduction2014年1期
- Asian Pacific Journal of Reproduction的其它文章
- Tuberculous orchitis mimicking a testicular tumor: A diagnostic dilemma
- Klinefelter syndrome and its association with male infertility
- Current insights into gonadotropic pituitary function in the polycystic ovary syndrome
- Investigation on leukocyte profile of periparturient cows with or without postpartum reproductive disease
- Tranexamic acid reduces blood loss during and after cesarean section: A double blinded, randomized, controlled trial
- Soluble fms-like tyrosine kinase-1 and vascular endothelial growth factor: Novel markers for unexplained early recurrent pregnancy loss
