Tuberculous orchitis mimicking a testicular tumor: A diagnostic dilemma
Seema Dayal, Alok Kumar, SP Singh, Archana Verma
1Department of Pathology, U.P. RIMS & R. Saifai Etawah, 206130 (U.P.), India
2Department of Forensic Medicine & Toxicology, U.P. RIMS & R. Saifai Etawah, 206130 (U.P.), India
3Department of Surgery, U.P. RIMS & R. Saifai Etawah, 206130 (U.P.), India
4Department of Neurology, U.P. RIMS & R. Saifai Etawah, 206130 (U.P.), India
Tuberculous orchitis mimicking a testicular tumor: A diagnostic dilemma
Seema Dayal1, Alok Kumar2*, SP Singh3, Archana Verma4
1Department of Pathology, U.P. RIMS & R. Saifai Etawah, 206130 (U.P.), India
2Department of Forensic Medicine & Toxicology, U.P. RIMS & R. Saifai Etawah, 206130 (U.P.), India
3Department of Surgery, U.P. RIMS & R. Saifai Etawah, 206130 (U.P.), India
4Department of Neurology, U.P. RIMS & R. Saifai Etawah, 206130 (U.P.), India
ARTICLE INFO
Article history:
Received 22 October 2013
Received in revised form 10 November 2013
Accepted 10 November 2013
Available online 20 January 2014
Tuberculosis
Orchitis
Seminoma
Ultrasound
Cytology
A 37-year old man presented with 5 months history of left scrotal mass and had underwent left orchidectomy following a presumptive diagnosis of testicular tumour. Histopathological diagnosis of testicular tuberculosis was subsequently made, which revealed a case of isolated TB orchitis. It signifies that the careful evaluation of patients with testicular mass is extremely significant for diagnostic accuracy, optimal treatment and avoiding unnecessary surgery in case of testicular tuberculosis. Simultaneously it will also help in early detection of testicular malignancies and vital for the clinicians to avoid negligence charges.
1. Introduction
Tuberculosis is one of the most important infection and ancient disease. It is estimated that about one third of the world population is infected with mycobacterium tuberculosis and most of the cases occur in Asia(55%) and Africa (31%) and rest in others[1]. Death in adult due to tuberculosis is more than any infectious disease [2]. With the background of very high prevalence, tubercular orchitis is not uncommon in developing country like India. Clinically, this condition may resemble epididymo-orchitis, sarcoidosis and malignancy [3]. As testicular biopsy is contraindicated in suspected case of malignancy. The diagnosis of tubercular orchitis can be achieved only on histopathological examination of resected testis and some time it comes with surprise. Tuberculous epididymo-orchitis is an important manifestation of genitourinary tuberculosis (GUTB) [4], which is the second most common form of extra pulmonary tuberculosis [5]. Genital tuberculosis other than tuberculous (TB) epididymitis is rare. Isolated TB orchitis without epididymal involvement is even more rare[6] .
Many cases coexist with pulmonary TB or tuberculosis of other parts of lower genitourinary system including bladder, ureter and prostate [7]. Isolated instances of tuberculous epididymitis or epididymo-orchitis is rare but when it occurs, a comprehensive assessment of the patient is mandatory[8]. Recent surge in the prevalence of TB worldwide linked to human immunodeficiency virus (HIV) pandemic has resulted in a concomitant increase in extrapulmonary TB of which GUTB accounts for up to 20% in endemic areas [9]. Isolated tuberculous orchitis is a rare entity and may mimic testicular tumours particularly in apparently healthy patients with no other clinical symptoms or signs, as in our case that presented as a testicular tumor. The following case is being presented on account of its rarity.
2. Case report
A 37 year old hetro sexual married male presented with a history of left scrotal mass of 4 months duration andone month’s history of low grade fever. The scrotal mass was smooth and firm accompanied by heavy testicular tender swelling. He complaint of discharge pain during urination and sex. There was history of weight loss, anorexia, hematuria and pyuria. General examination revealed thin built, poor nourishment and enlarged left inguinal lymph nodes. Chest X-rays was normal and did not reveal any metastasis.
Hematology examination revealed normocytic normochromic anemia, TLC was 21 800 with lymphocytosis. ESR was 60 mm in one hour. The placental alkaline phosphatase, alpha fetoprotein, HCG was within normal limits. Urine examination was positive for RBC and pus cells.
A diagnosis of testicular tumour was made and the patient underwent orchidectomy. Histopathology of the specimen (Figure 1 and 2) revealed testicular tissue with distorted architecture. It showed structure of testis with hylined blood vessel. Focal collection of caseative granular tissue surrounded by epithelioid cells, lymphocytes, langhan’s giant cell and fibrocytes (Figure 1 and 2). Finally, the diagnosis of tubercular orchitis was made.
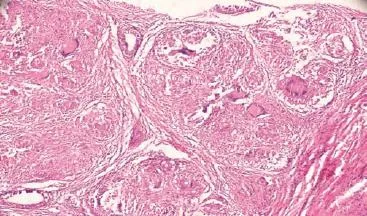
Figure 1. Low power microscopic photograph of tubercular orchitis showing giant cells, Langhans cells and testicular tissue.
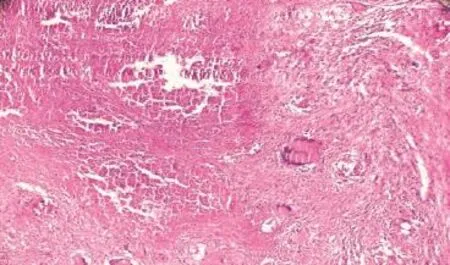
Figure 2. Photograph of tubercular orchitis showing necrotic material along with Langhans giant cells.
3. Discussion
Tuberculosis is a global epidemic with more than 2 billion of the world population infected [10]. Estimated 9 million new cases of TB were reported in 2007 and about 1.3 million deaths occurred among HIV-negative patients [11]. Tuberculosis can involve any organ, system in the body. While pulmonary tuberculosis is the most common presentation, extra pulmonary tuberculosis is also an important clinical problem [12]. Extrapulmonary tuberculosis (EPTB) is important because presentations in patients may simulate malignant tumours with diagnostic and treatment challenges. Several publications have reported various common sites of EPTB to include lymph nodes (The most common extra pulmonary site), GUTB, abdominal organs, CNS, skin and spine[13].
Genitourinary TB is the second most common site of involvement among extra-pulmonary TB [5] and may involve kidney, ureter, bladder or genital organs. Clinical symptoms usually develop after 10-15 years after primary infection. About ? of patient with GUTB have known history of TB, about half have normal chest radiography finding [14]. GUTB complicates 3%-4 % with pulmonary tuberculosis, active GUTB usually develop 5-25 years after primary pulmonary infection and usually encountered between the second and third decade of life[15].
About 28% of these patients will have isolated genital involvement[16]. The usual site of involvement is the epididymis, which occurs haematogenously or by a retrocanalicular haematogenous pathway from an infected prostate. If the infection goes unchecked, it can involve the testis. But, isolated involvement of testis is very rare. In a series of 96 cases of genital TB, Edward could not find any primary testicular TB, but all had the primary involvement of the epididymis [17].
The possible etiology of isolated tuberculous orchitis is that rarely the infection of the testis could be by hematogenous route rather than the usual direct extension from the epididymis. In one reported case of isolated TB orchitis, the patient presented with scrotal ulceration [18]. GUTB are usually symptomatic and manifested as increased frequency of urination, dysuria and painfull testicular swelling. Asymptomic patients are not common.
TB epididymo-orchitis is a common form of GUTB but when it is isolated, it may mimic testicular tumour. Seminoma and granulomatous orchitis occur in same age group with similar clinical presentation. Clinically seminoma and granulomatous orchitis can not be differentiated, as seminoma also present in same age group and there is no sensitive serological marker for seminoma is available.
Testicular tumour is rare among blacks and requires surgical removal with adjuvant chemoradiotherapy unlike testicular TB. In most developing countries including Asia and sub-Saharan Africa where the burden of TB is the highest, a complex intricate of poverty, overcrowding, malnutrition coupled with lack of newer diagnostic techniques have made adequate evaluation of patients prior to surgery difficult [19]. In the case presented, testicular and abdominal ultrasound with CT scan, and fine needle aspiration biopsy would have provided a guide to the management. Microscopy and culture negativity may not necessarily rule out TB Fine needle aspiration cytology (FNAC) has been reported to enhance diagnosis of testicular TB in conjunction with USS-CT scan[20].
It is important to note that in certain conditions orchitis is common in adult male e.g. spinal cord injury (SCI) patients and, therefore, both health professionals and SCI patients themselves tend to attribute testicular swelling to orchitis,with a consequent potential delay in the diagnosis of testicular tumours. Adults with spinal cord injury (SCI) are at greater risk of developing epididymo-orchitis than ablebodied individuals. Researchers from Leeds, U.K., found that 38.5% of SCI patients had suffered at least one episode of epididymo-orchitis[21] .
A SCI patient has been reported with testicular swelling who was initially prescribed ciprofloxacin for a presumptive diagnosis of acute bacterial orchitis, but who was subsequently shown to have a testicular tumour.
It is axiomatic that, for many tumours, early detection improves outcome, often with less intensive treatment. In contrast, the diagnosis of testicular tumours in this group of patients may be delayed because physicians and patients mistakenly attribute testicular swelling to orchitis, as indeed happened in this patient. Clinical history, physical examination, and ultrasound examination provide important clues as to the nature of testicular swellings in general. Ultrasound-guided fine needle aspiration (FNAC) of the testicular mass at the time of the first scan would have made the diagnosis of malignancy earlier. FNAC of the testis is a simple, quick, minimally invasive, and painless outpatient procedure [22].
In order to prevent delay in the diagnosis of testicular tumors in such SCI patients, following measures are proposed: (1) patients who develop testicular swelling should consult a physician immediately for clinical examination; blind antibiotic therapy should be avoided; (2) if clinical examination reveals a hard swelling and typical clinical features of acute urinary infection are absent, ultrasound scan of scrotum and if required, ultrasound-guided, FNAC should be performed to facilitate early diagnosis of testicular neoplasms; (3) education of SCI patients and their caregivers is also necessary in order to implement these recommendations [23].
Thus this diagnostic dilemma discussed as above, may result to inappropriate surgical procedure for a potentially curable medical illness. High index of suspicion, scrotal ultrasound and FNAC could be quite helpful in the diagnosis [20]. In addition to FNAC, polymerase chain reaction (PCR) when available has been shown to provide rapid detection of Mycobacterium tuberculosis (M. tuberculosis)[7]. Treatment with anti-tuberculous drugs in FNAC or PCR confirmed GUTB case may obviate the need for surgery and limit further organ damage. It is imperative that while striking a balance between cost and treatment, patients should be thoroughly investigated as the resultant infertility/ subfertility from orchidectomy may far outweigh the cost of investigation for a medically treatable condition such as tuberculosis. Moreover, correct diagnosis with timely and appropriate management will also save the clinicians from the charges of medical negligence.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Mandal AK, Chaudhary S. Tuberculosis. In: Text book of pathology. 1st ed. New Delhi: Avichal publication; 2010, p. 70.
[2] WHO. Global tuberculosis control, WHO report 2002. [Online]. Avaliable from: http:/www.who.in/ gtb/ publication.
[3] Gadgil NM, Ranadive NU, Sachdeva M. Granulomatous orchitis a case report. Indian J Urol 2001; 18: 92-94.
[4] Kapoor R, Ansari MS, Mandhani A, Gulia A. Clinical presentation and diagnostic approach in cases of genitourinary tuberculosis. Indian J Urol 2008; 24: 401-405.
[5] Wise GJ, Marella VK. Genitourinary manifestation of tuberculosis. Urol Clin North Am 2003; 30: 111-121.
[6] McAleer SJ, Johnson CW, Johnson WD. Tuberculous and parasitic and fungal infections of the genitourinary system. In: Campbell-Walsh urology. 9th ed. Philadelphia: Saunders Elsevier; 2007, p. 440.
[7] Wise GJ, Shteynshlyuger A. An update on lower urinary tract tuberculosis. Curr Urol Rep 2008; 9: 305-313.
[8] Shenoy VP, Viswanath S, D’Souza A, Bairy I, Thomas J. Isolated tuberculous epididymoorchitis: an unusual presentation of tuberculosis. J Infect Dev Ctries 2012; 6: 92-94.
[9] Das P, Ahuja A, Gupta SD. Incidence, etiopathogenesis and pathological aspects of genitourinary tuberculosis in India: A journey revisited. Indian J Urol 2008; 24: 356-361.
[10] Furlow B. Tuberculosis: a review and update. Radiol Technol 2010; 82: 33-52.
[11] Hanekom WA, Lawn SD, Dheda K, Whitelaw A. Tuberculosis research update. Trop Med Int Health 2010; 15: 981-989.
[12] Fanning A. Tuberculosis: Extra pulmonary disease. CMAJ 1990; 160: 1697-603.
[13] Ozvaran MK, Baran R, Tor M, Dilek I, Demiryontar D, Arinc S, et al. Extrapulmonary tuberculosis in non-human immunodeficiency virus-infected adults in an endemic region. Ann Thorac Med 2007; 2: 118-121.
[14] Mittal R. Disseminated tuberculosis with involvement of prostatea case report. Indian J Tubercul 2010; 57: 48-52.
[15] Hemal AK. Genitourinary tuberculosis. In: Sharma SK, Mohan A (eds.) Tuberculosis. New Delhi; Jaypee Brothers; 2001, p. 325-327.
[16] Wolf JS, McAninch JW. Tubercular epididymo-orchitis: Diagnosis by fine needle aspiration. J Urol 1991; 145: 836-838.
[17] Keyes EL Jr. Tuberculosis of the testicle: Observation upon 100 patients. In: Haynes IS. (ed.) New York: New York Surgical Society; 1905.
[18] Garbyal RS, Sunil K. Diagnosis of isolated tuberculous orchitis by fine-needle aspiration cytology. Diagn Cytopathol 2006; 34: 698-700.
[19] Orakwe JC, Okafor PI. Genitourinary tuberculosis in Nigeria; a review of thirty-one cases. Niger J Clin Pract 2005; 8: 69-73.
[20] Sah SP, Bhadani PP, Regmi R, Tewari A, Raj GA. Fine needle aspiration cytology of tubercular epididymitis and epididymoorchitis. Acta Cytol 2006; 50: 243-249.
[21] Mirsadraee S, Mahdavi R, Moghadam HV, Ebrahimi MA, Patel HR. Epididymo-orchitis risk factors in traumatic spinal cord injured patients. Spinal Cord 2003; 41(9): 516-520.
[22] Handa U, Bhutani A, Mohan H, Bawa AS. Role of fine needle aspiration cytology in nonneoplastic testicular and scrotal lesions and male infertility. Acta Cytol 2006; 50(5): 513-517.
[23] Vaidyanathan S, Hughes PL, Mansour P, Soni BM. Seminoma of testis masquerading as orchitis in an adult with paraplegia: proposed measures to avoid delay in diagnosing testicular tumours in spinal cord injury patients. The Sci World J 2008; 8: 146-156.
ment heading
10.1016/S2305-0500(14)60007-5
*Corresponding author: Dr. Alok Kumar, Additional Professor & Head, Department of Forensic Medicine & Toxicology, Faculty In-charge, Research Cell & Telemedicine Unit, Member Secretary of Research & Ethical Committee, UP Rural Institute of Medical Sciences and Research, Saifai, Etawah. -206130 (U.P.), India.
E-mail: drsalok@rediffmail.com
 Asian Pacific Journal of Reproduction2014年1期
Asian Pacific Journal of Reproduction2014年1期
- Asian Pacific Journal of Reproduction的其它文章
- Klinefelter syndrome and its association with male infertility
- Current insights into gonadotropic pituitary function in the polycystic ovary syndrome
- Investigation on leukocyte profile of periparturient cows with or without postpartum reproductive disease
- Tranexamic acid reduces blood loss during and after cesarean section: A double blinded, randomized, controlled trial
- Maternal outcome in multiple versus singleton pregnancies in Northern Tanzania: A registry-based case control study
- Soluble fms-like tyrosine kinase-1 and vascular endothelial growth factor: Novel markers for unexplained early recurrent pregnancy loss
