Is Retzius-sparing robot-assisted radical prostatectomy associated with better functional and oncological outcomes?Literature review and meta-analysis
Nji Isse Dirie , Gur Pokhrel , Wei Gun ,Mukhtr Adn Mumin , Jun Yng , Jkson Ferdinnd Msu ,Henglong Hu , Shogng Wng ,*
a Department of Urology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
b Department of Urology, The Second Affiliated Hospital of Zhejiang University School of Medicine,Hangzhou, China
c Department of Surgery, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
KEYWORDS Retzius-sparing;Radical prostatectomy;Robotics;Functional recovery;Positive surgical margins
Abstract Objective: To evaluate the efficiency, safety and clinical outcomes of Retziussparing robot-assisted radical prostatectomy(RS-RARP)in comparison with the standard RARP.Methods: A systematic search from Web of Science, PubMed, EMBase, Cochrane Library and Google Scholar was performed using the terms “Retzius-sparing”, “Bocciardi approach” and“robot-assisted radical prostatectomy”. Video articles and abstract papers for academic conferences were excluded. Meta-analysis of interested outcomes such as positive surgical margins (PSMs) and continence recovery was undertaken. A comprehensive literature review of all studies regarding Retzius-sparing (RS) approach was conducted and summarized.Results: From 2010 to 2017, 11 original articles about RS-RARP approach were retrieved. Of that, only four studies comparing the RS-RARP approach to the conventional RARP were comparable for meta-analysis.Faster overall continence recovery within 1 month after the surgery was noted in the RS group(61%vs.43%;p=0.004).PSMs of pT2 and pT3 stages were not significantly different between the groups (10.0% vs. 7.4%; p = 0.39 and 13.1% vs. 9.5%, p = 0.56,respectively). Of all the studies, only one reported sexual recovery outcomes after RS treatment in which 40% of the participants achieved sexual intercourse within the first month.Conclusion: Though more technically demanding than the conventional RARP,the RS technique is a safe and feasible approach. This meta-analysis and literature review indicates that RS technique,as opposed to the conventional approach,is associated with a faster continence recovery while PSMs were comparable between the two groups.The limitations of observational studies and the small data in our meta-analysis may prevent an ultimate conclusion. Future well-designed RCTs are needed to validate and confirm our findings.
Life expectancy and age-related diseases such as prostate cancer have increased over the last decades, especially in the developed world. The detection rate of organ confined and clinically inapparent prostate cancer specifically in younger patients has dramatically increased with the wide use of prostate-specific antigen (PSA) screening and highquality imaging techniques.Autopsies detected an increase in the prevalence of prostate cancer from 5% in men<30 years of age to 60%at the age of 80 years[1].However,the incidence varies according to different ethnic groups and geographic locations [2-4].
As detailed in the EAU 2017 guidelines, there are numerous approaches for the treatment and management of prostate cancer [5]. Radical prostatectomy either open or minimally invasive remains the gold standard for the treatment of localized and locally advanced prostate cancer [6]. Laparoscopic and robot-assisted radical prostatectomy have been linked to a shorter hospital stay, smaller surgical trauma and a fewer use of anesthetics [7].
The da Vinci?robot system (Intuitive Surgical Inc, Sunnyvale,CA,USA)has improved the ergonomics and provided an excellent 3D vision which allows surgeons to follow precise anatomic planes and avoid any thermal or mechanical damage to the neuro-vascular bundles (NVB).Cavernosal nerves are unmyelinated axons which are very sensitive to thermal energy; with that in mind, it has been highly advised not to use any thermal energy during any dissection near the NVB[8].The EndoWrist?instruments of the robotic arms can rotate up to 7°and are able to reduce tremor motions.These functions were specifically designed to assist the technically demanding urethrovesical anastomosis. Furthermore, several studies suggested that robotassisted radical prostatectomy (RARP) improved not only the surgical challenges but the oncological and functional outcomes as well [9,10]. Regardless of the surgical method used, the ideal common goals after radical prostatectomy(RP)are to achieve a better so called pentafecta,which are no early complications, no evidence of positive surgical margins (PSMs), sexual potency, continence recovery and free from biochemical recurrence [11].
Since the first report of RARP in 2001 [12], there have been many technical and technological advances.As stated in several studies, some techniques were associated with early continence and better sexual recovery after RP.These techniques included selective suture ligation of the dorsal venous complex (DVC) followed by a thermal division [13],preservation of the bladder neck, prostatic fascia (veil of Aphrodite) and accessory pudendal arteries [14-16].
In 2010,Galfano and his team[17]in Milan formulated a new technique named Retzius-sparing (RS) technique(posterior approach) which is entirely intrafascial and technically more challenging as opposed to the conventional robot-assisted radical prostatectomy (C-RARP). This new approach has resulted in the preservation of all anteriorly located structures in contrast to the conventional approach, such as endopelvic fascia, DVC (Santorini’s plexus), pubovesical ligaments and accessory pudendal arteries. To date, many institutions and centers have begun implementing this relatively new approach with comparable postoperative complication rates and a faster continence recovery as documented by Galfano et al. [17].
We conducted this meta-analysis and literature review to evaluate the effectiveness and postoperative outcomes of the Retzius-sparing robot-assisted radical prostatectomy(RS-RARP) technique in comparison to the conventional anterior approach.
2. Methods
2.1. Search strategy
A systematic search from Web of Science,PubMed,EMBase,Cochrane Library and Google Scholar using the terms“Retzius-sparing”, “Bocciardi approach”, and “robot-assisted radical prostatectomy” was performed to identify relevant studies published up to September 2017,comparing RS technique to the conventional anterior approach.Of that,only the studies published in the English language were retrieved for meta-analysis and literary review. Video articles and abstract papers for academic conferences and studies about the posterior approach but not sparing the Retzius space were all excluded. Metaanalysis of interested outcomes such as PSMs, continence recovery, and complication rates were undertaken. A comprehensive literature review of all studies regarding RS approach was conducted and summarized.
2.2. Data extraction
After a discussion of what was to be needed and excluded,the following data were extracted from each study: First author,publication year,the number of participants in each group,study design,characteristics of the participants and outcomes of interest.
2.3. Statistical analysis
A meta-analysis was performed to assess the overall outcomes of patients receiving RS-RARP as opposed to the conventional anterior approach. Studies were analyzed using the Review Manager software (RevMan v.5.3;Cochrane Collaboration, Oxford, UK). Since most of the studies did not provide the standard deviation (SD) of the preoperative and intraoperative continuous variables, the data were not applicable for analysis due to the limitations of Review Manager software. Postoperative dichotomous variables such as complication rates, PSMs, and continence recovery were statistically summarized as odds ratio (OR)and 95%confidence interval(CI).Meta-analysis was done by Random-effect models. In all statistical analysis, a p-value of <0.05 was considered statistically significant.
3. Results
Our literature search yielded 11 studies addressing RS-RARP technique: One randomized control trial (RCT), six observational studies, two case reports, one case series and one descriptive study [17-27]. We observed a lack of consistency among the parameters in the studies. Ultimately,four studies comparing RS procedure and the conventional anterior approach containing 250 cases in each group were comparable for meta-analysis [22,25-27]. Of all the variables provided in these four studies, only three postoperative dichotomous variables (continence recovery,PSMs and complication rates) were comparable for metaanalysis. The results of these studies are summarized in Table 1. Unfortunately, we could not find any data in the studies regarding the potency recovery after RS treatment for meta-analysis comparison.
Patient characteristics, study design, preoperative parameters, operative time, estimated blood loss, mean hospital stay and catheter length of all the studies concerning RS-RARP treatment approach (except two studies:One descriptive study and one study about the incidence of an inguinal hernia in RS-RARP treated patients [20,21]) are summarized in Table 2.
3.1. Surgical details
To begin the operation, the patient is set in a steep Trendelenburg position.The trocar placement of RS-RARP technique is principally similar to the C-RARP approach with a slight difference. Starting with 0°cameras, a 4 cm and U-shaped incision is made on the peritoneum covering of the seminal vesicles and the vas deferens. The vas is thermally dissected from the seminal vesicles and then transected, followed by the dissection of the seminal vesicles from the surrounding structures. As described in a video lecture by Foundation and Bocciardi [28], two trans-abdominal stiches were applied to the upper part of the previously opened peritoneum in order to expose the operative site and help with the dissection.Depending on the extent of the tumor,the plane is then selected,either extra-fascial, inter-fascial or intra-fascial for the prostate gland removal. The lateral pedicles are isolated and clipped using either titanium clips or Hem-O-lok. The dissection is then continued antegrade towards the apex of the prostate posteriorly until the membranous urethra is exposed. Tracing back to the base of the prostate, the bladder neck is isolated and detached from the beginning of the prostatic urethra. The dissection is then continued anteriorly towards the apex of the prostate gland without the need to open all anteriorly located structures.The specimen is removed after the transection of the membranous urethra from the apex of the prostate gland.Lastly,the camera is changed to 30°and then theurethrovesical anastomosis is performed (Fig. 1 and Fig. 2).
4. Meta-analysis of interested outcomes
4.1. Continence recovery
Overall continence recovery (completely dry or use of one pad for safety liner)within the first month after surgery was significantly faster in RS group as opposed to conventional anterior approach (random effect(RE): OR =3.53; 95%CI:1.48-8.40; p = 0.004, Fig. 3A). Completely dry (0 pad)participants were also significantly higher in RS group(RE: OR = 4.07; 95% CI: 2.03-8.14; p <0.0001, Fig. 3B).
4.2. PSMs
We analyzed three studies [22,26,27] in which the authors stratified the PSMs results according to pathological T staging. The results showed no significant difference between the two groups in both pT2 and pT3 stages (10.0% vs. 7.4%;p=0.39 and 13.1%vs.9.5%,p=0.56,respectively,Fig.4).
4.3. Complication rate
The overall complication rates were not statistically significant between the RS treatment and the conventionalanterior approach (RE: OR = 0.99; 95% CI: 0.39-2.55;p = 0.99, Fig. 5).
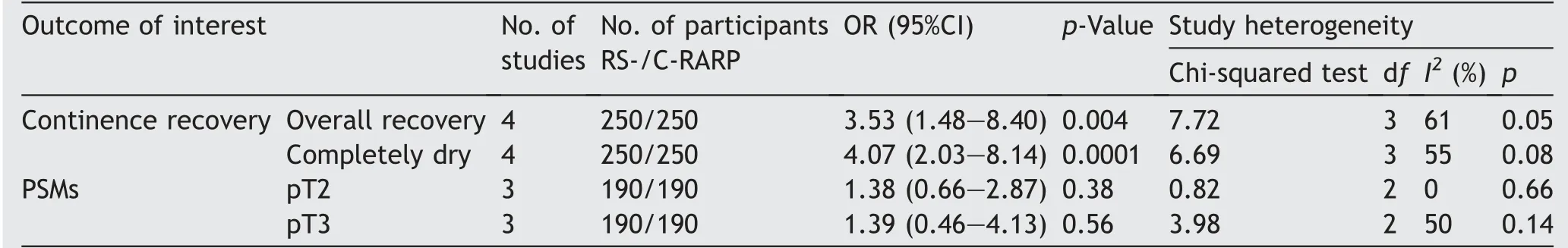
Table 1 Meta-analysis: Continence recovery and PSMs of RS-RARP vs. C-RARP.

Table: 2 Summary of all studies about Retzius-sparing robot-assisted radical prostatectomy.First author,year Study design Study participant Mean age(year)Operative time (min)Mean PSA level(ng/mL)Estimated blood loss (mL)Biopsy Gleason score Pathological stage Mean hospital stay (day)Mean catheter length (day)Group 1 Group 2 Group 1 Group 2 Group 1 Group 2 Group 1 Group 2 Group 1 Group 2 Group 1 Group 2 Group 1 Group 2 Group 1 Group 2 Group 1 Group 2 Galfano et al.,2010 [17]Case series 5-58-329-5.64-420-≤6 32-128----T1-5-----6.4 NA 10.6-78-10 T2 T3 Galfano et al.,2013 [23]Prospective 200-65-110-6.6-250-≤6 T1-68-7 & 4.5a -7-78-10 64--20 T2 826 T3 32--38 Lim 2014 et al.[22],Retrospective 50 50 65.7 66.2 117 141 12.8 10.5 299 260≤6 T1-41 4.8 5.5 NA NA 78-10 15 20 T2 9 8---------20 T3 9 12 Jenjitranant et al.,2016 [18]Case report 1-73-210-11.53-250-≤6-1--1-145 T1-1---------46 6-13-78-10 T2 T3--Raheem et al.,2016 [19]Case report 1-61-240-6.7-300-≤6 T1 4---78-10 T2-T3-Santok et al.,2016 [24]Retrospective 294-66.2-162-8.6-308-≤6 T1-191 6.3---78-10 149 T2-18 T3 103 Dalela et al.,2017 [25]RCT 60 60 61 61.5 NA NA 5.7 5.4 NA NA≤6 T1 40 NA NA NA NA 78-10 42 40 T2 20 13---40 T3---22 Eden et al.,2017 [26]Retrospective 40 40 63 65 200 223 5.4 6.8 200 200≤6-40 T1-37 2 2 8 14 78-10 T2-19-25 T3 Sayyid et al.,2017 [27]Prospective 100 100 61 62 120 144 8.75 7.07 100 100≤6 1 1 10.5 10.5 78-10 62 51≤T2 66 77 19 24≥T3 34 23 Group 1,Retzius-sparing robot-assisted radical prostatectomy;Group 2,conventional robot-assisted radical prostatectomy;NA,not available;PSA,prostate-specific antigen;-,no data;RCT, randomized control trial.a 7 days in their first 100 cases and 4.5 days in second 100 cases.
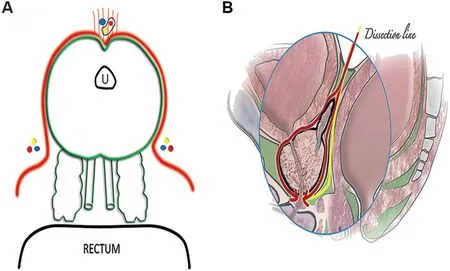
Figure 1 Dissection planes of Retzius-sparing robot-assisted radical prostatectomy(RS-RARP).(A)Transverse view of RS-RARP.Outsidetheredlineistheuntouchedareaofthesurgerycontaining the anterior compartment (dorsal venous complex, veil of Aphrodite, puboprostatic ligaments and the accessory pudendal arteries) and neuro-vascular bundles. (B) Sagittal section of the anatomic spaces crossed during the Bocciardi approach for RARP.The red line shows the intrafascial plane and the yellow line shows the extrafascial plane,with the Denonvillier’s fascia in the middle (black). U, urethra. (Reproduced with the permission of Elsevier,License number:4155670913161).
5. Discussion
RARP is one of the most frequently performed procedures in the field of surgical oncology. The 2016 annual report of Intuitive Surgical Inc. stated that da Vinci?prostatectomy(dVP)grew from 60 000 procedures in 2014 to 70 000 in 2016 in the United States alone. Outside the United States, the number also grew from 65 000 in 2014 to 92 000 in 2016,indicating that solely in the year of 2016;more than 160 000 RARP procedures were completed globally [29], which signifies the substantial growth of this single procedure and the need of innovative changes to improve the outcomes.
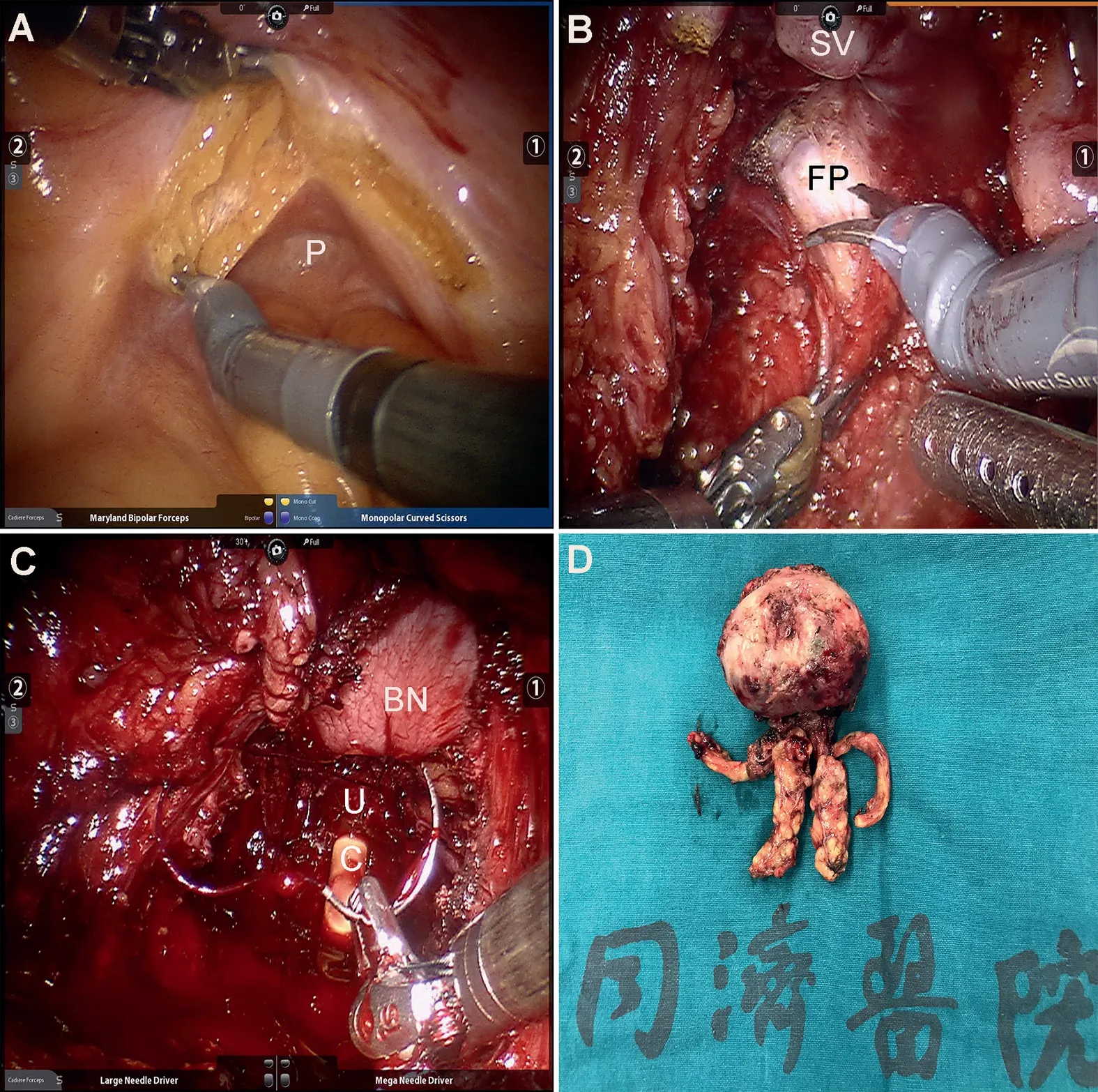
Figure 2 Retzius-sparing robot-assisted radical prostatectomy technique. (A) 4 cm incision on the peritoneum; (B)Fascial plane selection; (C) Urethro-vesical anastomosis; (D)Specimen(prostate).BN,bladder neck;C,catheter;FP,fascial plane; P, peritoneum; SV, seminal vesicle; U, urethra.
5.1. Operative time, estimated blood loss and hospital stay
This review included 11 studies about the RS technique(Bocciardi approach). The estimated blood loss and the operative time of RS-RARP approach ranged between 100-420 mL and 110-329 min, respectively. The mean hospital duration of those who received RS-RARP ranged between 2 and 7 days [23,26,27] while the mean time to remove the catheter ranged between 8 and 13 days [17,18,27].
5.2. Complications
Our meta-analysis demonstrated comparable overall complication rates between the RS and the conventional approaches(10.8%vs.9.6%,p=0.58).Galfano et al.[17]documented two cases of bladder perforation in their first case series study.In another cohort of 200 patients by the same team, only two complications were recorded: One prostatic fossa bleeding and one acute abdomen(caused by a bowel hernia)in which both cases required re-operation [23]. Since ureters run posterolateral to the bladder wall which is very close to the operative site,the most serious complication reported in the studies came from a clip that was accidentally applied to the ureter and finally resulted in ureteral obstruction [26].Fortunately,most of the investigators recognized this danger and warned to avoid it during RS-RARP surgery[17,26].
In respect to the exact technique employed,a 4 cm peritoneum incision was utilized throughout the procedure which at the end of the surgery was complitely sealed with sutures.This smaller incision reduces surgical trauma while also enhancing postoperative recovery period, in contrast to the much larger incision used during C-RARP approach. On the other hand,this small and posteriorly located approach brings new technical challenges that can influence intraoperative and postoperative outcomes.Due to these challenges,some investigators could not complete some of their RS cases and decided to convert into the more familiar conventional anterior approach.Galfano et al.[17]converted two of their first five RS cases,while Dalela et al.[25]and Eden et al.[26]reported 5%and 7.5%conversion rates,respectively.
In a study comprising 294 cases of RS-RARP by Santok and colleagues[24],participants were divided into three groups according to prostate size (Group 1: <40 mL; Group 2:40-60 mL; Group 3: >60 mL). Investigators found a higher blood loss, transfusion rate and increase of console time in Group 3 when compared with Groups 1 and 2.In addition to that,some investigators safely performed simultaneous RSRARP and nephron sparing surgery(NSS)[19],and according to Jenjitranan et al. [18] kidney transplanted patients can also receive RS-RARP technique without any technical challenges except some slight changes of port placement.
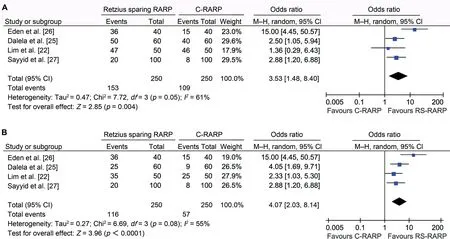
Figure 3 Continence recovery (RS-RARP vs. C-RARP). (A) Overall continence recovery. (B) Completely dry. RS-RARP, Retziussparing robot-assisted radical prostatectomy;C-RARP,conventional robot-assisted radical prostatectomy;M-H,Mantel-Haenszel.
In regards to the learning curve and mastery of this relatively new technique, two cohort studies were performed to investigate the influence of the learning curve on the outcomes.Lim et al.[22]found significant console time difference between their first and second 25 cases while Galfano et al. [23] documented overall PSMs of 32% vs.19%(p <0.039) between their first and second 100 cases,respectively.
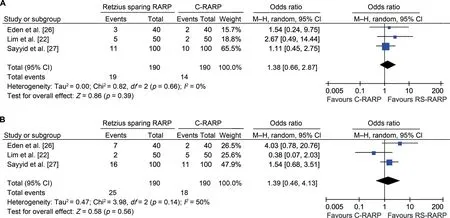
Figure 4 Positive surgical margins of RS-RARP vs.C-RARP.(A)pT2(pathological stage).(B)pT3(pathological stage).RS-RARP,Retziussparing robot-assisted radical prostatectomy;C-RARP,conventional robot-assisted radical prostatectomy;M-H,Mantel-Haenszel.
Speaking the correlation between the mastery and the outcomes, a new study by Schiffmann et al. [30] after 10 years of experience with RARP procedure, researchers divided their patients into three groups based on the year operated(Group 1:2007-2010,Group 2:2011-2012,Group 3: 2013), and then observed if patient characteristics, selection, and outcomes have changed overtime as the surgeon’s experience grew [30]. Their results showed significant overtime increase of PSA level,D’Amico high-risk patients, biopsy and pathological Gleason scores, pelvic lymph node dissection (PLND) rates, and more non-organconfined diseases. All these findings are believed to be the result of the surgeon’s experience. As the surgeon becomes more experienced which depends on the number of cases he/she operates then the surgical restrictions reduce overtime, meaning as his/her experience grow the confidence of taking more challenging cases grows as well.
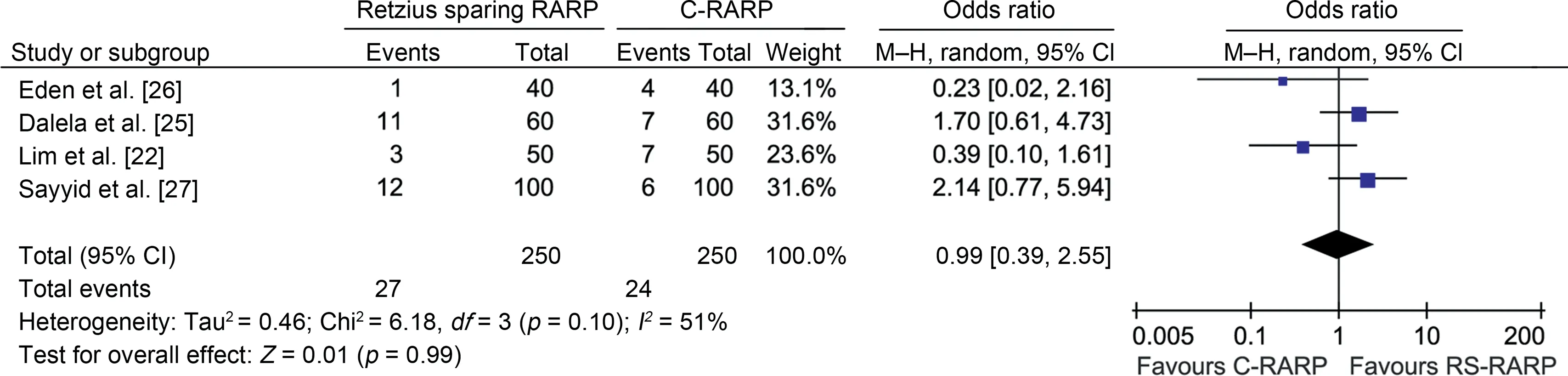
Figure 5 Complication rates of RS-RARP vs. C-RARP. RS-RARP. Retzius-sparing robot-assisted radical prostatectomy; C-RARP,conventional robot-assisted radical prostatectomy; M-H, Mantel-Haenszel.
5.3. PSMs
One of the main concerns of postprostatectomy is the PSMs.PSMs are key predictors of the biochemical recurrence(BCR),and they are unfavorable pathological findings such as extraprostatic extension and seminal vesicle or bladder neck invasion. BCR is defined as a relapse of PSA (PSA >0.2 ng/mL)after the surgery [31]. There are several factors that influence PSMs including prostate volume and the BMI, both having a tendency to increase the PSMs [32]. Furthermore,high-volume surgeons have been reported to reduce margin positivity[33].Nevertheless,there is still an on-going debate about the superiority of one surgical approach to the other in regards to the PSMs. Some authors reported similar PSMs results between open and RARP approaches[32]while others encountered higher PSM rates in minimally invasive approaches [34]. In a study by Jo and colleagues [35], they reported 14.48% of apical margins and 18.65% of PSMs in other sites of those received RARP.They also found a strong association between the clinical tumor stage and the biopsy Gleason score with the BCR free survival and pathologic outcomes in patients found positive apical margins.
Our current meta-analysis revealed that PSMs were not significantly different between the standard RARP and RS-RARP. Similarly, in a two-case series study about RSRARP, one by Galfano et al. [23], and the other by Santok and colleagues [24], containing 200 and 294 cases respectively, found overall PSMs of 25.5% and 22.7%, respectively.On the other hand, some authors have recognized slightly higher incidence of PSMs involvement in the anterior location of those who received RS approach compared to the conventional anterior approach. Lim et al. [22] and Eden et al. [26] found 8% vs. 0% and 5% vs. 0% in the anterior region of the RS group when compared to the conventional approach,respectively.Based on these above findings,some investigators have advised against RS technique if the tumor involves in the anterior region. But arguably these findings could be related to the learning curve of this relatively new approach and hopefully improved over time as showed in the C-RARP. Nevertheless, some other investigators did not report these similar findings in their study [27].
5.3.1. Continence recovery
A major advantage of RS-technique is that it allows for a fast continence recovery time as described in most of the studies concerning RS-RARP. In our meta-analysis, 1 month after the surgery, the overall continence recovery was faster in RS group when compared to the C-RARP approach(61%vs.43%;p=0.004).Perhaps this is a direct result due to the nature of this approach, which spares many important structures in the anterior of the prostate gland such as pubovesical ligaments, puboprostatic fascia, NVB and Santorini plexus(DVC)[20].The importance of these abovementioned structures to continence recovery was discussed in various studies [36-38].
Of the three successful RS cases reported by Galfano et al.[17] two patients used one safety pad during the first 24 h after the removal of the catheter while the third patient did not need any pad at all. In another case series of RS technique with 200 participants by the same investigators, an overall continence recovery of 91% within 7 days after catheter removal was recorded [23]. Similarly, Santok and colleagues [24] found an overall continence recovery of 93.9% after 1-year follow-up in their cohort of 294 cases.
We believe that even better continence recovery outcomes could be achieved in the near future as the surgeon’s experience and techniques grow towards this relatively new approach. Perhaps this is because knowing how experience and better understanding have changed the standard RARP continence outcomes. For instance in a new study by Fossati et al. [39] they compared surgical outcomes of three surgeons based on their experience with the RARP procedure,and found about 60%continence recovery at the initial while as surgeon’s procedures hit >400 cases, the continence recovery grew considerably up to 90%.
5.3.2. Potency recovery
Since 1982 when Walsh and Donker [40] described the concept of neuro-vascular bundles (NVB) and their associations with the sexual recovery,there have been many other investigators documented many different anatomical structures and advocated their preservation in order to enhance potency recovery after radical prostatectomy. These concepts become even more significant in the recent years since more younger patients are diagnosed with prostate cancer in which better functional outcomes is hugely important as cancer control. There are many techniques that have been reported to have a better potency recovery in relation to the others such as unilateral and bilateral nerve sparing techniques, retrograde and antegrade approach, intra- and interfascial dissections and so on[41].
Of all the studies regarding RS treatment approach,only Galfano and his team [17] reported results about the potency recovery while the rest of the investigators did not include any data concerning sexual recovery outcomes. In their first case series of Galfano et al. [17], of the three successful cases one patient experienced a full erection within 24 h after removal of catheter,and in another cohort by the same investigators, of the 77 cases that received bilateral intrafascial nerve-sparing, 40% (31/77) achieved sexual intercourse within the first month [17,23].
In conclusion, we can clearly see that most of the investigators of RS-RARP poorly reported sexual recovery outcomes after the surgery while they heavily investigated continence recovery and PSM outcomes. It seems future well-designed studies specifically focusing on potency outcomes after RS treatment are required.
5.3.3. Inguinal hernia (IH) and RS-RARP
Higher incidence of IH after retropubic prostectomy is another well-documented matter. In a meta-analysis study published by Zhu and colleagues [42] reported a 15.9%incidence of IH after RARP compared to 6.7% after laparoscopic radical prostatectomy(LRP)while Yamada et al.[43]recorded 14% (43/307) of IH incidence after RARP during 2-year follow-up.They showed that the incidence of the IH was significantly related to the surgeon’s experience (High volume[≥40 cases]vs.Low volume[<40 cases]were 9%vs.1%, respectively) and incontinence at 3 and 6 months after the surgery. The incidence rate has the possibility of being lower if some preventive technical methods are undertaken as Shimbo and colleagues [44] reported.
In addition,RS-RARP is associated with a lower incidence of IH. Chang et al. [21] documented 3.7% (11/298) incidence of IH in the RS technique group versus 7.8%(42/541)found in the C-RARP approach. The correlation of this may be due to the preservation of numerous structures located in the anterior of the pelvic wall.
6. Conclusion
The literature on the RS-RARP is still in a premature stage,due to the lack of well-designed studies with large participants and longer follow-up period. Based on the existing data, the approach is safe and feasible, though more technically demanding than the C-RARP approach.
This meta-analysis and literature review indicates that RS technique, as opposed to the conventional anterior approach, is associated with faster continence recovery in the first month after the surgery while PSMs and complication rates are similar in both groups.Unfortunately,most of the investigators did not provide detailed data regarding sexual recovery outcomes after RS-RARP for a conclusion.On the other hand, let’s not forget that there are many other predictors that can influence the functional and oncological outcomes other than the technique utilized such as patient’s age, preoperative international prostate symptom score and sexual health inventory for men score,the existence of diabetes mellitus, surgeon’s experience,the extent of the tumor and many others.
The limitations of observational studies, short follow-up time of the studies and the smaller data in our meta-analysis may prevent an ultimate conclusion. Future well-designed RCTs are needed to validate and confirm our findings.
Author contributions
Study concept and design:Najib Isse Dirie,Shaogang Wang.Data acquisition: Najib Isse Dirie.
Data analysis: Gaurab Pokhrel, Jun Yang, Jackson Ferdinand Masau.
Drafting of manuscript: Najib Isse Dirie.
Critical revision of the manuscript: Gaurab Pokhrel, Wei Guan, Mukhtar Adan Mumin, Jun Yang, Jackson Ferdinand Masau, Henglong Hu, Shaogang Wang.
Conflict of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2019年2期
Asian Journal of Urology2019年2期
- Asian Journal of Urology的其它文章
- Asynchronous abdominal wall and sigmoid metastases in clear cell renal cell carcinoma:A case report and literature review
- Compliance in patients with dietary hyperoxaluria: A cohort study and systematic review
- Dose escalation of external beam radiotherapy for high-risk prostate cancer-Impact of multiple high-risk factor
- Effect of warm bladder irrigation fluid for benign prostatic hyperplasia patients on perioperative hypothermia, blood loss and shiver: A meta-analysis
- Beyond prostate, beyond surgery and beyond urology: The “3Bs” of managing non-neurogenic male lower urinary tract symptoms
- Systemic treatment for metastatic prostate cancer
