Neonatal Staphylococcal Scalded Skin Syndrome: A Case Report
Yuan-Xia Zou,Jia-Yu Zhang,Xiao-Xiu Ye,Hui Zhou,Run Li,Gui-Ping Li*
1Department of Newborn Medicine, Hospital Affiliated to Southwest Medical University,Luzhou, Sichuan, China; 2School of Clinical Medicine,Yunnan University of Traditional Chinese Medicine,Kunming,Yunnan,China.
Abstract Objective: To summarize the clinical features, diagnosis, and treatment of neonatal staphylococcal scalded skin syndrome (SSSS). Methods: The clinical data with SSSS was analyzed, and the related literature was reviewed.Results: The acute onset of the disease was characterized by generalized erythema, epidermis exfoliation, skin non-touch,radial chapping around the mouth,and positive Nissl sign.The culture of binocular secretions and neck exudates showed Staphylococcus aureus and was diagnosed as SSSS.According to the results of drug sensitivity of secretions and exudates, vancomycin was selected for anti-infective treatment, and skincare and symptomatic support were given simultaneously.The child was cured and discharged after ten days of treatment. Conclusion:SSSS belongs to neonatal acute and critical illness.Improving etiological examination and timely targeted anti-infective treatment is the key to correct diagnosis and recovery.
Keywords:Newborn;Staphylococcal scalded skin syndrome;Staphylococcus aureus;Mastitis
Introduction
Neonatal staphylococcal scalded skin syndrome(SSSS)is an acute and severe infectious skin disease known as neonatal exfoliative dermatitis, Staphylococcal toxic epidermal necrolysis, Rittervon Ritterschein disease,Ritter disease and Lyell disease, and staphylococcal necrolysis of the epidermis.Studies have found that the incidence of SSSS is increasing year by year [1],mainly manifested as generalized skin erythema on the whole body,loose bullae,and large exfoliation[2,3].It is more common in infants and children, mainly contact infection, but also It is intrauterine infection,and the disease progresses quickly.It can cause a nosocomial outbreak in the neonatal ward [4,5], and the mortality is high [6,7].Recently,a child with SSSS was admitted to our neonatal intensive care unit and recovered and discharged after active treatment.The report is as follows.
Clinical information
The patient was male, age twenty-two days.He was admitted to the hospital for "skin rash for four days,aggravated with skin rupture for one day".Five days before admission, the mother had a fever with the highest temperature of 39 ℃, who was diagnosed as mastitis.Therefore, the infant was changed from breastfeeding to formula feeding.Four days before admission, a little red rash appeared on the forehead,accompanied by a little yellow secretion in the eyes and red skin around the mouth.Parents ignored the symptoms,and no remission was observed.Since then,red spots gradually appeared on the neck,accompanied by a few white corn-like size spots,not higher than the skin surface."Bingbai Liquid" was diluted 1:1 with warm water and wipe it out by themself".One day before admission, the family members found that the child's skin around the mouth was flushed with a little yellow exudate, the skin on the neck was flushed, and the white spots of corn-like size increased to the size of mung beans, not higher than the skin.The child was crying and restless, and the family member realized that the child's skin temperature was high, and the highest temperature was 37.3 ℃.The child was admitted to the hospital on July 21, 2020, because of his condition's worsening.On the day of admission,the child was irritable, crying, and refusing to touch.The frequency of stools increased,and the quality was thin(10+ times/day), and physical examination was appended.Birth history: G3P2, 38+5 weeks gestation,birth weight of 3.7 kg.Apgar scores at 1 min, 5 min and 10 min after birth were all 10 points.Exclusive breastfeeding was given after birth,and no abnormality in breast milk volume and urine was found.The mother was healthy during pregnancy and had no family history of similar related diseases.
Physical examination revealed no abnormalities in the heart,lungs,abdomen,and nervous system.Skin examination:the face was scattered with light-red skin rash, a large number of purulent secretions were seen in both eyes, both eyelids were red and swollen, and conjunctival hyperemia was evident.Flushing was found around the mouth,and yellow crusts can be seen around the nose and mouth,showing radial cracks.The skin rash on the neck has been further enlarged, with small white blisters about 1 ~ 1.5 cm in diameter.No clear blister fluid was found.Part of the blister ruptured with a little yellow exudate.The skin at the base was flushed, and the Nissl sign was positive.The skin around the anus was flushed.A little erythema was scattered on the trunk, and no unmistakable rash was observed(Figure 1 A-D).
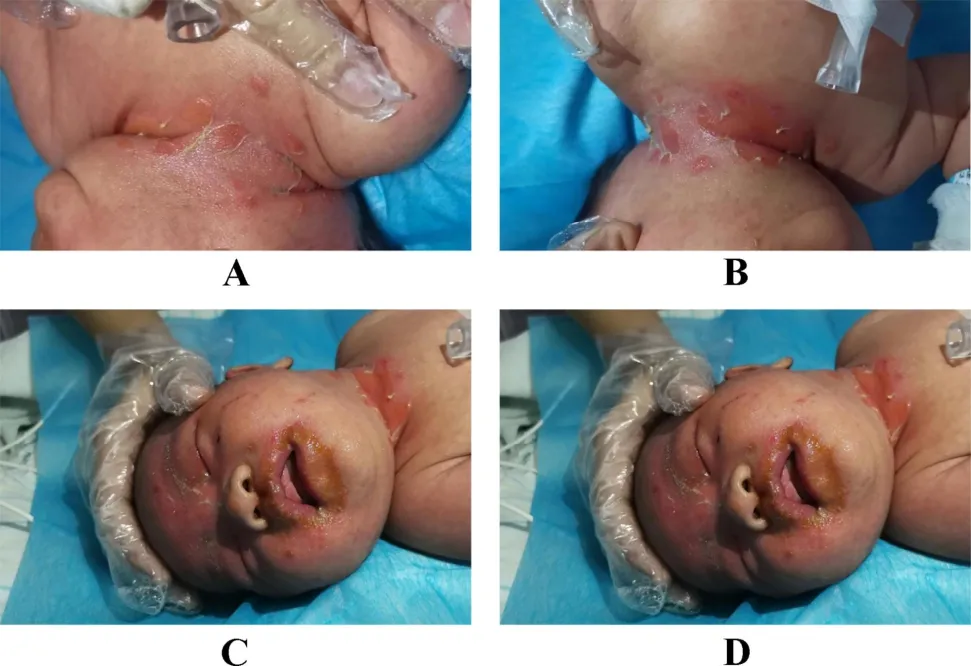
Figure 1.A-D:The clinical manifestations of the child on admission.
Auxiliary examination:blood routine examination:WBC 14.39 × 109/L, N 28.9%, L 48.4%, RBC 4.3 ×1012/L, HB 142g/L, HCT 39.9% and PLT 340 × 109/L.No abnormality was found in liver function, kidney function, PCT, and CRP after admission, and no abnormality was found in reexamination after one week of treatment.Gram staining of secretions in both eyes: more epithelial cells were seen, and Gram-positive cocci were found.2 days after admission, the etiological examination showed that Staphylococcus aureus was found in binocular secretion culture and in cervical secretion culture, all were sensitive to oxacillin sodium and vancomycin.Two blood cultures were negative.Allergen test showed no allergy to milk protein.Fundus examination revealed no abnormalities in both eyes.The auditory brainstem response examination showed that both ears were normal.
The preliminary diagnosis was SSSS on admission, and the diagnosis was further confirmed after the secretion culture results were returned.
Treatment and outcome: single-room isolation was performed immediately after admission.After treatment with oxacillin sodium 25 mg/kg q6h for two days, the child's facial and neck skin lesions were improved.Desquamation and exuviation were visible.However, there was diffuse flushing on the skin all over the body, the back was evident, and a few white spots were seen on it, which was not hindered by the touch.New flushing of the skin was seen in both armpits, elbows of upper limbs, bilateral groin area,and around the anus.The doctor asked the medical history again.After the mother was diagnosed with mastitis, she applied to milk to the child's eyes and rash.Combined with the child's binocular secretions and neck secretions, the cultures all returned staphylococcus aureus.The diagnosis was further confirmed as SSSS, so oxacillin sodium was discontinued and changed to vancomycin 10 mg/kg q8h anti-infective treatment for seven days.
Skin care: adding kangfuxin soluion 120 mL 1:1 to warm water for seven days.Mupirocin ointment 0.1g bid was given for external rubbing.Oxygen therapy was performed on the wound.Recombinant human epidermal growth-factor topical solution 2 mL qd topical was used to promote the growth of skin lesions and other skin care.After the eyes were cleaned with normal saline, the eyes were given tobramycin drops of 0.02 mL q4h.Deep hydrolyzed milk was used to feed the patient child, and oral montmorillonite suspension and“Live Combined Bifidobacterium”was used to regulate intestinal flora.On the 4th day after admission, the child's skin flushing improved significantly, and no evident herpes or exudate was observed.Exuviation and desquamation were observed,a little desquamation was observed on the 8th day,and the whole-body skin returned to normal on the 10th day.A follow-up one week after discharge showed no recurrence(Figure 2).

Figure 2.Skin condition after healing.
Discussion
In this case, the mother had a definite history of fever before the disease's onset, and mastitis was diagnosed.The child was exclusively breastfed after birth,and the mother changed to milk powder after mastitis diagnosis.When there was a little skin rash on the child's face and a little secretion from the eyes, the mother applied breast milk to the skin rash on the child's eyes and face.Since then, the disease of the child gradually worsened and progressed rapidly.However, the common pathogenic bacteria of mastitis are Staphylococcus aureus and Streptococcus, so the child has a clear history of contact infection, and it is not difficult to make a diagnosis based on symptoms and signs.The disadvantage is that the early selection of antibiotics is not significant.After two days of treatment, new erythema and white blisters appear again.The effect of vancomycin in anti-infection treatment is noticeable.Secondly, samples of breast milk or secretions from mothers and other immediate family members were not available for culture.
The pathogenic bacteria of SSSS are mainly Staphylococcus aureus of coagulase-positive phage group II,type 71,which can also be caused by type 55.Other pathogens are Streptococcus, hemolytic Streptococcus, and so on.The bacterium can produce epidermolysis A and epidermolysis B (also known as detoxification).Among them, epidermolysis A acts on desmosomes or acts as a superantigen to cause superficial separation of epidermal keratinocytes,leading to skin loosening and intra-epidermal blisters[8].Positive Nissl's sign can be found clinically.
The main diagnostic features of SSSS are generalized erythema and scalded epidermis exfoliation.Further diagnosis can be made by sampling and culture of secretions or skin biopsy of diseased areas [9].Therefore, it needs to be differentiated from toxic epidermal necrolysis (TEN),bullous epidermolysis, neonatal impetigo, and desquamative erythroderma. The typical manifestations of TEN are painful local erythema with the rapid spread.The relaxed bullae and epidermal exfoliation occurred on the basis of erythema, and the Nissl sign was positive.Drug allergies, systemic epidermal inflammation mostly cause it, and necrosis is deeper than SSSS, accompanied by more exudation,obvious pain, and slower relief.The patient's general condition is wretched, especially the mucosal erosion of mouth, eyes, and respiratory tract, which occurs mostly in adults.Epidermolysis bullosa is a group of rare polygenic inherited vesicular skin diseases characterized by blister formation resulting from slight friction.Newborn pustule, also known as "infectious pustule disease",is commonly known as"yellow water boil".It manifests as sudden blisters or bullae on the face, trunk, and limbs, with pea to walnut size, thin wall, and no significant blush around.Desquamative erythroderma is more common in infants 1-3 months and is manifested as diffuse flushing throughout the body,accompanied by a small grayish-white bran scale.Greasy grayish-yellow scales were found on the scalp,eyebrows,and nose wing.The above four diseases can be distinguished from SSSS through clinical observation and bacteriological or pathological skin lesions results.
Neonatal immune function and the kidney's ability to remove toxins are low, so the incidence rate is higher than that of adults.Prevention is similar to other neonatal skin diseases.The baby's skin is delicate.First, parents should pay attention to keeping the baby's skin clean, wash hands before touching the newborn, and change clothes frequently.Secondly,contact with newborn babies by skin infected persons should be avoided, and appropriate environmental temperature and moderation should be maintained.
Antimicrobial therapy is key to the treatment of SSSS.Timely use of sensitive and effective antibiotics can inhibit and kill Staphylococcus aureus, reduce toxin production, and block further disease development.Penicillins,such as nafcillin or oxacillin,can be used as emergency treatment drugs.If methicillin-resistant Staphylococcus aureus(MRSA)is suspected,antibiotics that cover MRSA should be used,such as vancomycin, linezolid, etc.Clindamycin is considered the drug of choice to prevent bacterial ribosomes from producing exotoxins.In terms of topical skincare, a 2% Mupirostar ointment bid can be applied externally, and fundamental fibroblast growth factors can promote skin growth.Besides,glucocorticoids may be used in combination with severe cases.Patients with severe infection can be intravenously injected with gamma globulin in cooperation with anti-infection treatment.Due to the increase of insignificant water loss because of skin peeling, attention should be paid to symptomatic and supportive treatment such as fluid and electrolyte supplementation.In clinical work, a reasonable treatment plan should be made according to children's individual situation to prevent and reduce the occurrence of complications.
- Nursing Communications的其它文章
- The application progress of auricular therapy in diabetes
- Effects of Modern Online and Traditional Offline Exercise Programs on the Frailty, Physical function, Emotional, and Social Support on Chinese Community-Dwelling Frail Older Adults: A Randomized Clinical Trail
- Comparison of Status of Mental Health of Male Nursing Students between China and Korea: A Cross-Sectional Study
- Current Situation Analysis of Nursing Students' Professional Attitudes and Employment Intentions during COVID-19 Pandemic

