Calorie restriction or dietary restriction: how far they can protect the brain against neurodegenerative diseases?
Tayana Silva de Carvalho
Abstract Finding the correct nutritional intervention is one of the biggest challenges in treating patients with neurodegenerative diseases. In general, these patients develop strong metabolic alterations, resulting in lower treatment efficacy and higher mortality rates.However, there are still many open questions regarding the effectiveness of dietary interventions in neurodiseases. Some studies have shown that a reduction in calorie intake activates key pathways that might be important for preventing or slowing down the progression of such diseases. However, it is still unclear whether these neuroprotective effects are associated with an overall reduction in calories (hypocaloric diet) or a specific nutrient restriction (diet restriction). Therefore, here we discuss how commonly or differently hypocaloric and restricted diets modulate signaling pathways and how these changes can protect the brain against neurodegenerative diseases.
Key Words: Alzheimer’s disease; diet therapy; dietary intervention; epilepsy; fasting;glucose restriction; hypocaloric diet; multiple sclerosis; Parkinson’s disease; stroke
Introduction
Epilepsy is one of the oldest known neurodiseases, at which time the treatment was based on lower food intake (Magiorkinis et al.,2014). Almost a century later, other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s disease, multiple sclerosis,and stroke, have been reported in middle-aged and elderly people.Unfortunately, these diseases still lack pharmacological and nonpharmacological treatments. Therefore, recent studies have started to consider calorie restriction and dietary restriction as possible candidates for being added to the therapy as a non-pharmacological treatment (Pasinetti et al., 2007; Srivastava and Haigis, 2011; de Carvalho et al., 2019a; Verrotti et al., 2020).
However, due to the complexity of these diseases, it is not easy to modify the dietary intake of neurologic patients, since > 20% of epileptic patients, 12.6–59.8% of Alzheimer’s disease (AD) patients,17.2–40% of Parkinson’s disease (PD) patients, 8% of multiple sclerosis(MS) patients, and 6–62% of stroke patients are undernourished or at risk of undernutrition on the onset of neurological symptoms(Crepin et al., 2009; Foley et al., 2009; Sheard, 2014; Redondo Robles et al., 2019). During the disease time course, these patients normally develop eating and swallowing problems, resulting in marked weight loss, nutritional deficiencies, poor prognosis, stronger neurological symptoms, and lower therapeutic efficacy (Foley et al., 2009; Bouziana and Tziomalos, 2011; Sheard, 2014).
On the other hand, eutrophic patients, who restricted their calories or one kind of nutrient either before the onset of the disease or during the treatment, had a better prognosis. This occurs because restrictive diets are able to activate important metabolic pathways associated with protection (Manzanero et al., 2011; de Carvalho et al., 2019a, b, 2020; Phillips, 2019).
Therefore, as summarized in Figure 1, in the absence of undernutrition, calorie restriction or dietary restriction can be considered as a therapy for all the above-mentioned neurodiseases.Nevertheless, it is unknown which restrictive diet can be better applied for each neurodisease, in which a restrictive diet is more effective for reducing neurological symptoms, and which signaling pathways these diets can use to promote neuroprotection. Based on these questions, the present study aimed to discuss the possible neuroprotective effects of these diets across different neurodisease conditions.
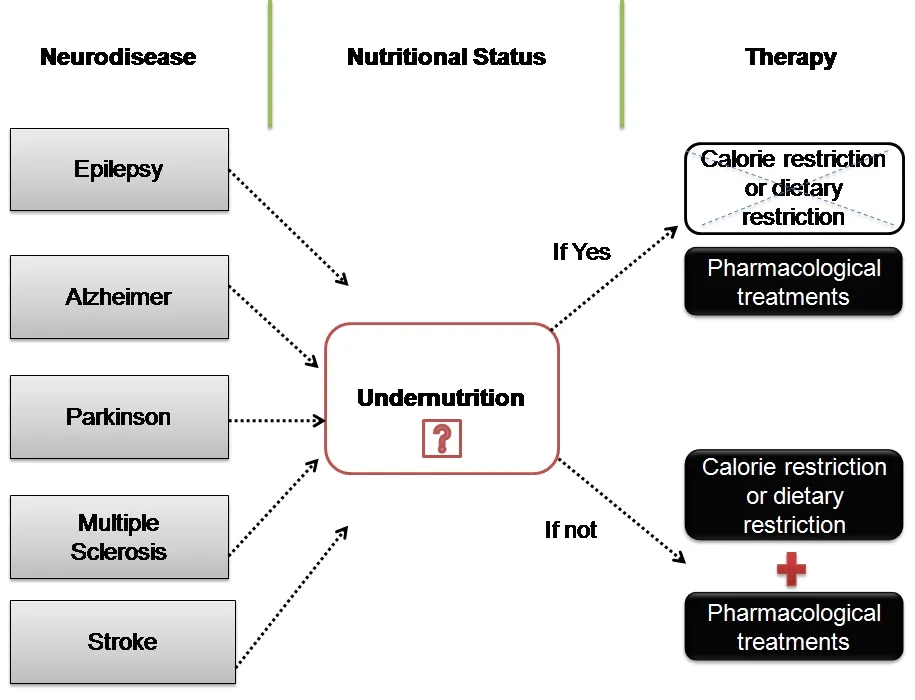
Figure 1 |An illustrative relationship between dietary intake and neurological diseases.Neurological diseases such as epilepsy, Alzheimer, Parkinson, multiple sclerosis, and stroke can activate important catabolic pathways that result in undernutrition. In this context, a reduction of nutrients is harmful, might not show protective effects, and must be excluded from the non-pharmacological strategy. However, patients with unaltered nutritional conditions can undergo this approach, being a useful strategy for applying together with the current pharmacological interventions for such diseases.
Search Strategy and Selection Criteria
Studies cited in this review published from 2000 to 2021 were searched on the PubMed database using the following keywords:Neurological diseases, undernutrition, Alzheimer’s disease,Parkinson’s disease, multiple sclerosis, epilepsy, calorie restriction,dietary restriction, and neuroprotection.
Understanding the Differences between Calorie Restriction and Dietary Restriction
Before discussing the potential neuroprotective effects of calorie restriction or dietary restriction on neurodiseases, it is important to conceptually define them (Table 1).
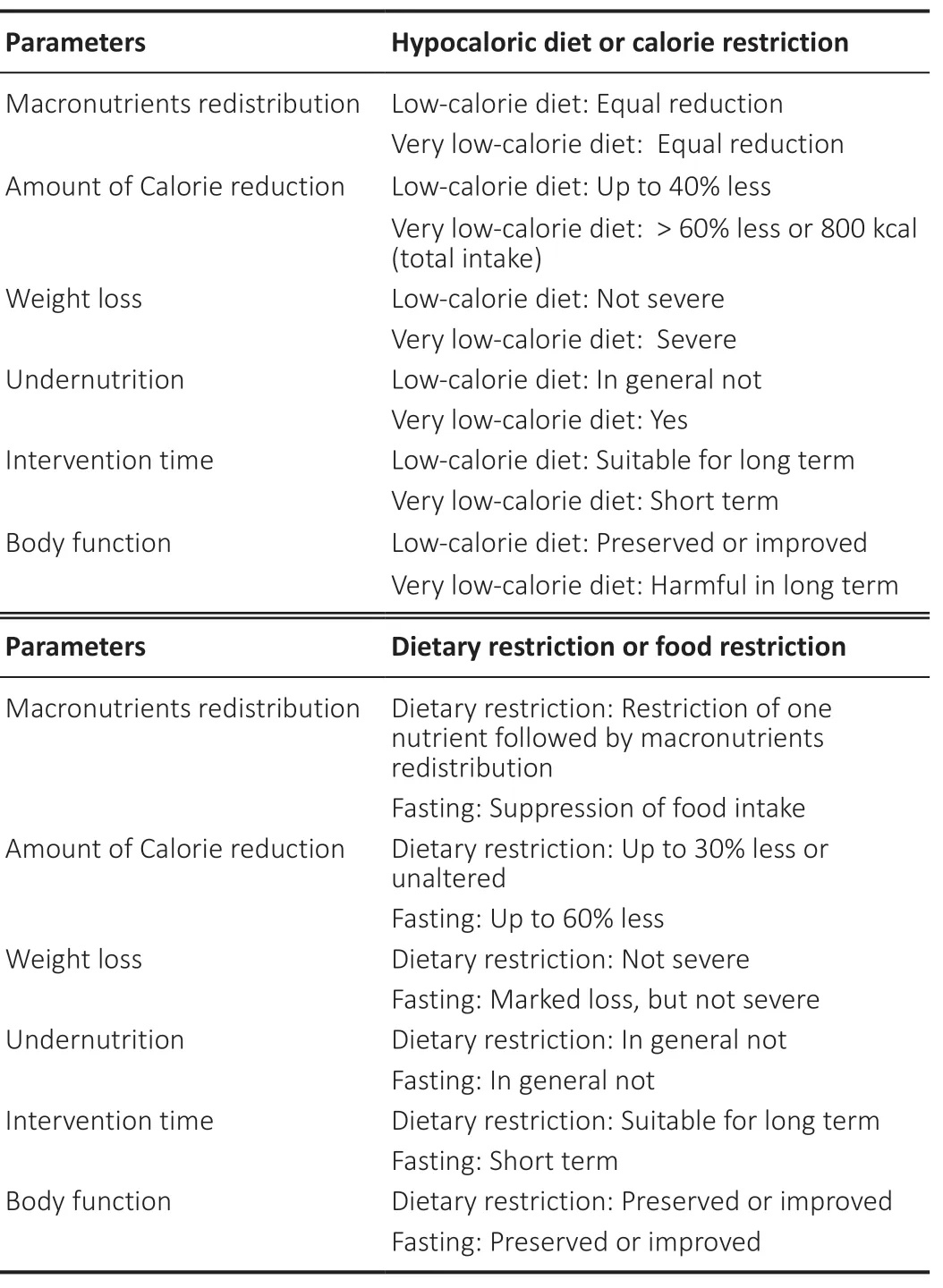
Table 1 |Summary of nutritional changes promoted by hypocaloric diet or dietary restriction
Calorie restriction diet (hypocaloric diet) can be primarily described as an overall reduction in the total amount of calories from all macronutrients (Atkinson, 1989). However, this overall reduction in calories can be subclassified as a “l(fā)ow-calorie diet” or a “very lowcalorie diet.” In which, a “very low-calorie diet” represents an intake of less than 800 kcal. This lower intake is mostly associated with severe nutritional depletion, resulting in a metabolic risk, namely undernutrition (Atkinson, 1989). A “l(fā)ow-calorie diet,” instead, has a moderate reduction (up to 40% of the total amount of calorie intake)that keeps offering enough nutrients for the whole body function,being normally namely as calorie restriction or hypocaloric diet(Atkinson, 1989). These concepts are summarized in Table 1.
Dietary restriction, however, has a broader definition, consisting of a restriction of one particularly nutrient (macro or micro) or a periodic feeding restriction (fasting) (Lee et al., 2016). Under controlled conditions, dietary restriction does not lead to undernutrition,but it can induce marked changes in metabolism in the long term.This is because a restriction of one nutrient leads to macronutrient redistribution, reducing the number of nutrients that can be harmful to a particular disease or health condition. On the other hand, fasting can reduce up to 60% of the total amount of food intake, but this needs to be applied in a short period of time to not endanger whole body function (Lee et al., 2016). These concepts are summarized in Table 1.
Interestingly, even when the definition is mixed, particularly between very low dietary intake and dietary restriction, several previous studies found a high association between lower calorie intake and reduced neurological disease progression (Love, 2005; Pasinetti et al.,2007; Srivastava and Haigis, 2011; Van Cauwenberghe et al., 2016;de Carvalho et al., 2020). These associations are discussed in detail in the following sections.
The Role of Calorie Restriction and Dietary Restriction on the Neurological Symptoms
Regardless of nutritional status, during the aging process or at the onset of different neurodiseases, it is common to observe changes in brain volume, adenosine triphosphate production, neuropeptide levels, inflammatory and neurotransmitter activity, reactive oxygen species formation, neuronal loss, and plaque deposition (Landi et al., 2016; Moore et al., 2018). In the face of these alterations, it is clear that changes in diet need to be carefully applied to preserve brain function. In addition, there are two important aspects to be considered: (1) how far dietary interventions can protect against neurological symptoms and (2) how these interventions play a role in the course of epilepsy, Alzheimer’s disease, Parkinson’s disease,multiple sclerosis, and stroke. In this context, this section summarizes and discusses what is already known about the impact of calorie restriction and dietary restriction on the progression of neurological symptoms.
Among to the other neurodiseases, epilepsy is the one, who has the closest and oldest relation with food intake as a treatment. Fasting and lower meat intake were the first recommended treatments for this disease (Magiorkinis et al., 2014). Several studies have shown that fasting, ketogenic, and enriched medium-chain triglyceride diets when combined with pharmacological treatment can inhibit seizure susceptibility, increase seizure threshold, and have anticonvulsive effects (Greene et al., 2001; Verrotti et al., 2020). Likewise, calorie restriction can also reduce seizure occurrence, but this intervention might be effective only in a short time, once that even in lower amounts, there are some macronutrients that need to be completely avoided during the seizures. Interestingly, both calorie and dietary restriction can induce a fast response after being imposed, showing that the metabolic shift has a huge impact on seizure control.However, considering the number of improvements promoted by dietary restriction in this particular disease, it is worth noting that this approach is the most effective intervention against seizures when compared to calorie restriction, as summarized in Table 2 (Stafstrom,2004).
Systematic reviews have shown that lower intake of carbohydrates and hypocaloric diets can protect against cognitive decline and cortical thickness changes (Smith and Blumenthal, 2016; Staubo et al., 2017; Bianchi et al., 2019). Similarly, a hypoprotein diet could also successfully promote neuroprotection, as described in Table 2 (Van Cauwenberghe et al., 2016). However, it is still necessary to clarify how long it is possible to maintain these positive effects.
In a Parkinson disease model, animals under calorie restriction for 6 months had better motor activity, higher basal ganglia response,and greater neuronal survival (Maswood et al., 2004). A protective effect was also observed in animals fed with a hypoprotein diet(Table 2) (Wang et al., 2017). However, a hypoprotein diet also has a detrimental role in the pharmacological therapy for PD, as this diet can interfere with levodopa absorption (Wang et al., 2017). This influence can directly impair motor function and leads to dyskinesia in a long-term (Wang et al., 2017).
In patients with MS, a reduction of up to 22% in calorie intake leads to lower depressive scores (Fitzgerald et al., 2018). Likewise,intermittent fasting can delay neurodegeneration by reducing demyelination, inflammation, and axonal damage processes (Table 2)(Katz Sand, 2018; Foolad et al., 2019). However, in this case, dietary restriction seems to play a more effective role in symptoms than calorie restriction.
In stroke models, calorie and dietary restriction interventions are associated with better neurological recovery, spatial learning, and cognitive improvements, followed by reduced brain infarction after short-or long-term dietary intervention (Roberge et al., 2008; Ran et al., 2015; de Carvalho et al., 2019a, b, 2020). On the other hand,several studies using severe restriction (0–2% protein or 60% calorie less intake) showed impaired brain and neurological recovery even after short-time diet treatment (Bobyn et al., 2005; Smith et al.,2014; Alaverdashvili et al., 2015, 2017, 2018). Therefore, we can conclude that the level of restriction and intervention time are two critical points to be considered before choosing between calorie restriction and diet restriction in stroke models.
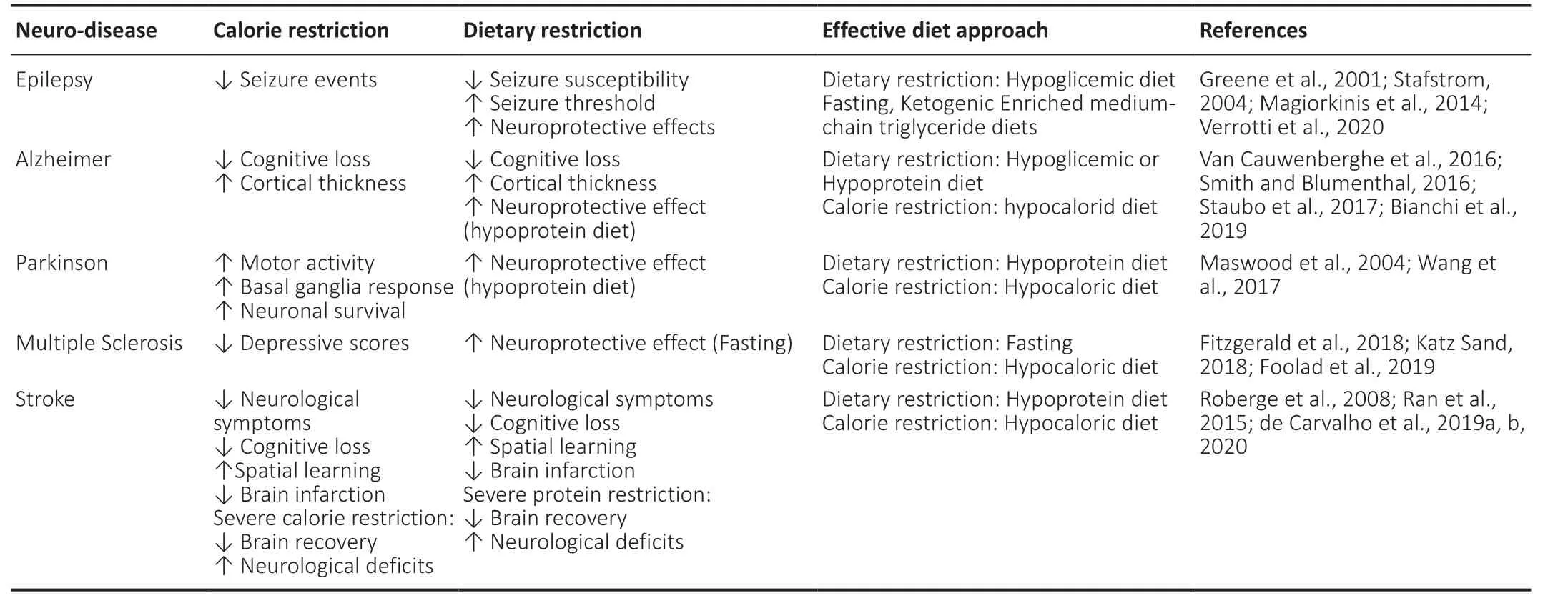
Table 2 |Neurological symptoms improvements induced by calorie or dietary restriction in Epilepsy’ disease, Alzheimer’s disease, Parkinson’s disease,Multiple sclerosis’s disease and Stroke’s disease
Even so, in the anabolic stage, calorie restriction and dietary restriction can efficiently reduce the neurological symptoms in all the neurodiseases mentioned above (Table 2). This improvement indirectly increases the quality of life and reduces the progression of the disease, which is an important achievement in diseases without cure. However, it is not surprising that in all the aforementioned diseases, significant weight loss was observed during the diet interventions. This is a side effect that has to be deeply considered,because neurodiseases can lead to catabolism, particularly at later time points. Consequently, at this stage, all the nutrients will be recruited to maintain cell survival instead of offering energy to fight against neurological symptoms. Therefore, this metabolic shiftdemands more knowledge about the involved signaling pathways, in order to judge how far calorie restriction and dietary restriction can be safely applied in each neurodisease.
Neuroprotective Signaling Pathways Activated by Calorie and Dietary Restriction: Differences and Similarities
Beyond body weight control, calorie and dietary restriction can also induce further molecular changes that might be decisive for the progression of neurodisease. However, it is important to understand how differently or similarly these restrictive diets can change the signaling pathways in every neurodisease before deciding on one(Table 3).
Mechanistically, several studies have shown that calorie restriction activates sirtuins. Upregulation of this protein optimizes metabolism.At the brain level, this optimization reduces neuronal loss, rescues blood flow, maintains cellular metabolism, inhibits inflammatory pathways, and stimulates antioxidant activity. Several studies have shown that sirtuins play an important role in AD, PD, Epilepsy’s disorder, and stroke diseases by inducing neuroprotection (Srivastava and Haigis, 2011; Zhang et al., 2018; Chuang et al., 2019; Foolad et al., 2019). However, de Carvalho et al. (2019a) showed that the activation of sirtuins is not exclusively done by calorie restriction,as was believed before, but also by moderate reduction of protein intake (dietary restriction). This latter result indicates that Sirtuin upregulation can be a common protection route offered by calorie and dietary restriction.
Similarly, all the above-mentioned diseases showed an upregulation of brain-derived neurotrophic factor after calorie or dietary restriction intervention (Maswood et al., 2004; Van Cauwenberghe et al., 2016; de Carvalho et al., 2020; Li et al., 2020). Along with this upregulation, increased energy expenditure in strategic brain regions and greater neurotransmitter activities were observed (Rothman et al., 2012). This improvement might slow down brain damage and delay the progression of the disease.
Nevertheless, it is possible that calorie restriction and dietary restriction activate more neurodisease-related pathways. For example, in epilepsy disease, most of the protective effects are attributed to increased ketosis promoted by glucose restriction(Greene et al., 2001; Verrotti et al., 2020). Under ketosis, cells are less stimulated, resulting in lower frequencies of hyperpolarization,glutamatergic and adrenergic receptor activation, higher stimulation of GABA receptors, and increased expression of glutamic acid decarboxylase isoforms (Stafstrom, 2004). At the molecular level, it was found less DNA methylation, reactive oxygen species formation,and increased growth factors (brain-derived neurotrophic factor and glial cell line-derived neurotrophic factor) activity and autophagy (Li et al., 2020).
In AD models, experimental and clinical studies have shown that calorie restriction increases the production of antioxidants and anti-apoptotic proteins, boosts histone deacetylase activity,reduces accumulation of amyloid-β plaques, activates astrocytes,controls insulin pathways, raises brain-derived neurotrophic factor levels, increases DNA repair, and inhibits the mechanistic target of rapamycin pathway (Van Cauwenberghe et al., 2016). These alterations are detrimental to neuronal survival, tau phosphorylation,and Aβ-induced cell death (Van Cauwenberghe et al., 2016).However, a typical rebound effect induced by lower calorie intake was reported by McGuire and Ishii (2018), who observed that patients with mid-life obesity and a later life weight loss had an inefficient leptin transport up to the blood-brain-barrier. This lower level of leptin reduces the insulin-degrading enzyme, decreases Aβ clearance and production, increases tau phosphorylation, and impairs hypothalamic activity. All these alterations can trigger a chain reaction, leading to cognitive loss (McGuire and Ishii, 2016).In terms of dietary restriction, a reduction in protein intake (dietary restriction) was mostly associated with lower DNA damage, but not with further protective signaling pathways (Van Cauwenberghe et al., 2016). In contrast, a hypoglycemic diet induces synaptogenesis,impairs the microbiome associated with AD-related Aβ pathogenesis,upregulates neurotrophic factors, reduces neurotoxicity and amyloid deposition, and downregulates tau-bearing neurons by controlling the insulin signaling pathways (Bianchi et al., 2017; Cox et al., 2019).In this context, AD patients can benefit from both diet interventions unless they show nutritional disturbances such as undernutrition.
In the same direction, PD animals under calorie restriction showed numerous improvements, such as increased dopaminergic neuron survival in the substantia nigra, followed by higher levels of dopamine, dopamine metabolites, brain-derived neurotrophic factor (1/2-fold), and glial cell line-derived neurotrophic factor (3-fold) at the striatum level (Maswood et al., 2004). These positiveeffects are potentially supported by increased ghrelin activity in the hypothalamus, mitochondrial biogenesis, and pAMPK activity,particularly in dopamine neurons (Bayliss et al., 2016). However,in the case of fasting, ketone bodies also helped to preserve mitochondrial adenosine triphosphate function, inhibit interleukine 1β, reduce insulin resistance, and increase the production of shortchain fatty acid bacteria production (Jackson et al., 2019).
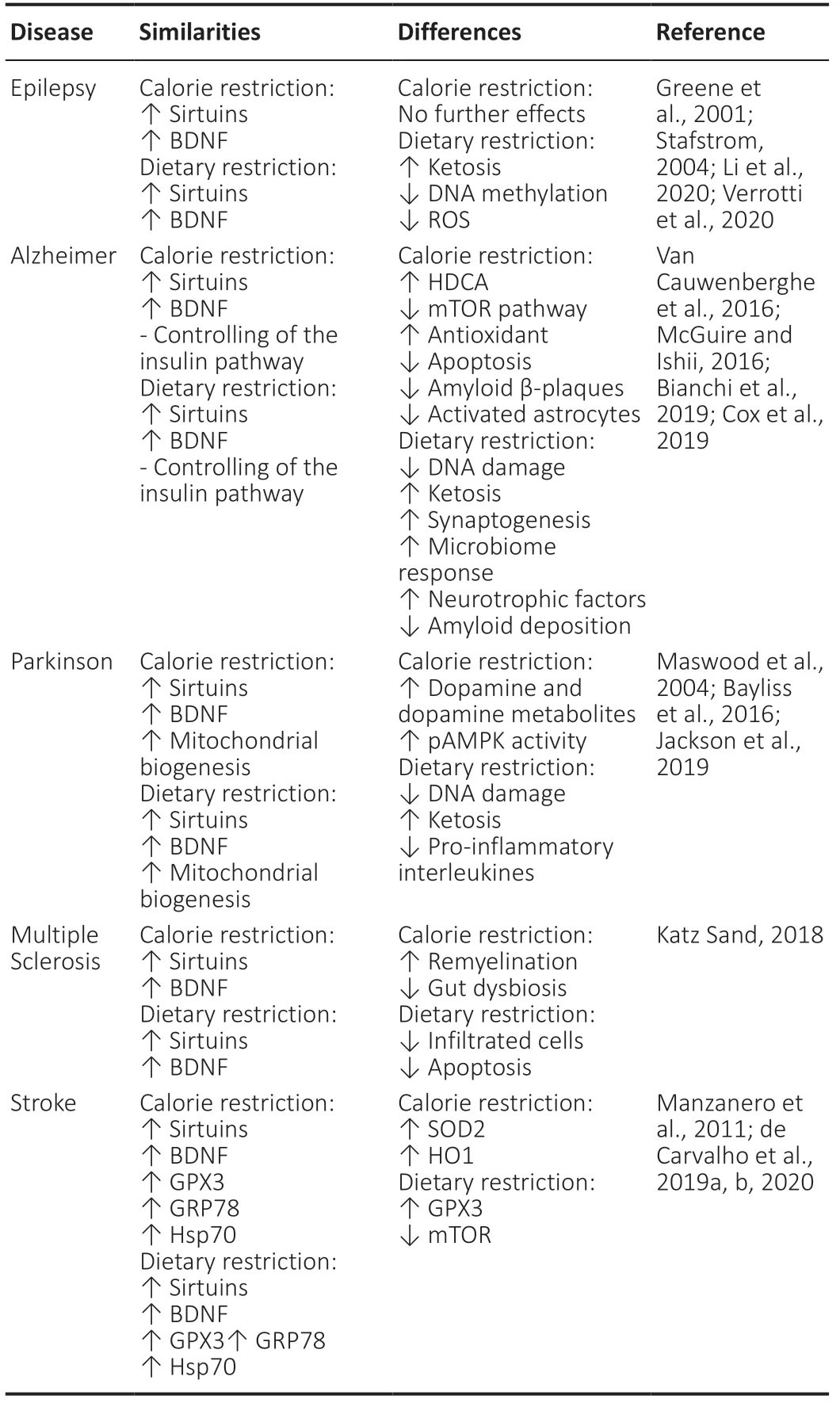
Table 3 |The summary of signaling pathways activated by calorie or dietary restriction in Epilepsy’ disease, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis’s disease and Stroke’s disease: similarities and differences
Surprisingly, in MS, calorie and dietary restriction activate specific pathways that are beyond metabolism and are more antiinflammatory-related (Katz Sand, 2018). An experimental study recently proved that calorie restriction can increase oligodendrocyte generation in animals cotreated with cuprizone, resulting in increased remyelination potential (Mojaverrostami et al., 2020).Calorie restriction reduces gut dysbiosis, resulting in lower levels of pro-inflammatory markers and lipopolysaccharide production and decreased cross-reactive immunity (Riccio and Rossano, 2015).After fasting, lower levels of infiltrated immune cells in the spinal cord, decreased CD4+T cell accumulation, and apoptosis events in oligodendrocytes, and increased Treg and corticosteroid production were observed (Katz Sand, 2018; Bai et al., 2021). Therefore, the dietary restriction can develop a more sophisticated protection using the metabolic shift to control the anti-inflammatory effects.
In stroke models, the upregulation of glucose-regulated protein 78, heat shock protein 70, Glutathiona peroxidase-3, superoxide dismutase-2, and heme oxygenase-1 protein expression as well as the inhibition of mechanistic target of rapamycin have been associated with the neuroprotective effects induced by calorie restriction and dietary restriction (Manzanero et al., 2011; Ahn et al., 2018; de Carvalho et al., 2019a, 2020). In this condition, it is believed that calorie restriction and dietary restriction increase brain resistance against ischemia. These diets, per se, are already an insult that can teach brain cells to function under a limited nutrient source(Manzanero et al., 2011). In post-conditioning intervention, only a single study showed that calorie restriction can induce positive effects such as increased neurogenesis and angiogenesis, reduced inflammation, and moderately improved motor function in the long term (de Carvalho et al., 2020). However, it is important to highlight that stroke patients develop dysphagia, and this symptom can be a huge limitation for the use of any kind of restrictive diet after stroke.Based on the above studies, it is possible to affirm that calorie restriction and dietary restriction can effectively teach the brain to better use the energy source for activating key signaling pathways associated with neuroprotection (Table 3). However, considering that the brain needs to work under a limited nutrient source under these diets, a long-term intervention might be difficult to compensate for the nutrient deficit. From this point, the brain starts to show signs of exhaustion and catabolism (Bouziana and Tziomalos, 2011;Manzanero et al., 2011; de Carvalho et al., 2019b). This means that this narrow line can be easily crossed if the patients have 1) some previous nutrient deficiency before the diet intervention or the onset of the disease or 2) became undernourished during the treatment.Consequently, the signaling pathways shift from a protective to an apoptotic direction.
The other critical point is related to the pharmacological intervention,because in the case of PD and ED, dietary restriction needs to be part of the treatment, which is an unavoidable intervention. However, for AD, MS, and stroke diseases, it is important to also consider the effect of medications on appetite, gastric function, body weight, nutrient absorption, insulin metabolism, gut alterations, and mood changes(Hansen et al., 2008; Wang et al., 2017; Klotz et al., 2019). Once that,all these alterations can automatically compromise the nutritional status and limit any restrictive intervention. In addition, the current nutritional status of patients needs to be considered, avoiding severe nutritional deficiencies.
In terms of time, the literature still lacks information regarding the safest intervention time. Once that, most clinical studies have only performed short-term interventions with a limited number of patients. Likewise, experimental studies have mostly used healthy animals for up to a few weeks of intervention. However, considering the high risk of catabolism, it might be dangerous to use restrictive diets up to later stages or for long term use. Thereafter, these diets can be applied differently based on the stage of the disease, genetic factors, and current metabolic conditions.
In terms of prevention, calorie restriction can be a successful option for retarding the onset of stroke, Alzheimer’s disease, and Parkinson’s disease. For this assertive, there are two possible explanations: (1)the brain is less exposed to harmful nutrient amounts, reducing the power of metabolism in the development of those diseases and (2)after calorie restriction, the brain might have a fast recovery or slow disease progression, as the brain already knows how to behave under an injury.
In terms of symptom control, restriction of one specific nutrient seems to be more effective for epilepsy, Alzheimer’s disease,Parkinson’s disease, MS, and stroke. Single nutrient restrictions can more specifically modulate brain activity, reduce excitation, modify membrane composition, activate non-aerobic pathways, prevent cell death, and improve cell response. However, it is important to highlight that most of these positive effects are associated with lower glucose and protein intake, because both diets can similarly control insulin pathways, as described in Table 3. This tight relationship between glucose metabolism and neurodegenerative diseases has received increasing attention, particularly after recent findings that proved that AD can be similarly classified as brain diabetes (type 3 diabetes) (de la Monte, 2017). A few years later, this insulin signaling dysfunction was also found in PD, Epilepsy’s disorder, and stroke patients, making this theory more widely applied to other diseases(Ruiz-Argüelles et al., 2018; Holscher, 2020; Sekar et al., 2020; Chang et al., 2021).
In the case of treatment efficacy, dietary restriction seems to have a more efficient effect than calorie restriction. This applies,particularly for ED and PD, as they need to restrict nutrients as a rule for controlling the level of brain discharge (seizures) and to increase the medicament response (ED and PD) (Wang et al., 2017; Li et al.,2020).
In summary, calorie and dietary restriction can be considered an optimal non-pharmacological approach for supporting neurodisease treatment or for retarding the onset of these diseases. Even though, a single diet modification cannot completely prevent their development, this approach was more “neuroprotective” than overall calorie restriction. Additionally, further studies must be conducted to better understand how far these diets can keep the positive metabolic response and when could be the best time-point to impose this diet as a preventive approach.
Author contributions:The author confirmed sole responsibility for the following: study conception and design, literature analysis and interpretation,manuscript preparation, and approved the final version of the manuscript.
Conflicts of interest:The author declares no conflicts of interest.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons AttributionNonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
?Article author(s) (unless otherwise stated in the text of the article) 2022. All rights reserved. No commercial use is permitted unless otherwise expressly granted.
- 中國神經(jīng)再生研究(英文版)的其它文章
- Motor neuron replacement therapy for amyotrophic lateral sclerosis
- Monodelphis domestica: a new source of mammalian primary neurons in vitro
- Vascular inflammation in the central nervous system
- Proper progression of neurogenesis relies on a defined pattern of SUMOmodified proteins
- Elucidating the pathological mechanisms of neurodegeneration in the lethal serpinopathy FENIB
- Glial cell line-derived neurotrophic factor in brain repair after focal ischemic stroke