lmpact of body mass index in elderly patients treated with laparoscopic liver resection for hepatocellular carcinoma
Maria Conticchio,Riccardo Inchingolo,Antonella Delvecchio,Francesca Ratti,Maximiliano Gelli,Massimiliano Ferdinando Anelli,Alexis Laurent,Giulio Cesare Vitali,Paolo Magistri,Giacomo Assirati,Emanuele Felli,Taiga Wakabayashi,Patrick Pessaux,Tullio Piardi,Fabrizio di Benedetto,Nicola de’Angelis,Javier Brice?o,Antonio Rampoldi,Renè Adam,Daniel Cherqui,Luca Antonio Aldrighetti,Riccardo Memeo
Maria Conticchio,Antonella Delvecchio,Riccardo Memeo,Unit of Hepato-Pancreatic-Biliary Surgery,“F.Miulli” Regional General Hospital,Bari 70021,Italy
Riccardo lnchingolo,Interventional Radiology Unit,“F.Miulli” Regional General Hospital,Bari 70021,Italy
Francesca Ratti,Luca Antonio Aldrighetti,Unit of Hepatobiliary Surgery,San Raffaele Hospital,Milano 20132,Italy
Maximiliano Gelli,Departement de Chirurgie Viscérale,Gustave Roussy Cancer Campus Grand Paris,Paris 94800,France
Massimiliano Ferdinando Anelli,Javier Brice?o,Unit of Oncologic and Pancreatic Surgery,Hospital University Reina Sofía,Cordoba 14004,Spain
Alexis Laurent,Nicola de’Angelis,Assistance Publique-H?pitaux de Paris,Department of Digestive and Hepatobiliary Surgery,Centre Hospitalier Universitaire Henri Mondor,Créteil,Paris 94000,France
Giulio Cesare Vitali,Service of Abdominal Surgery,Poliambulanza Foundation,Brescia 25124,Italy
Paolo Magistri,Giacomo Assirati,Fabrizio di Benedetto,Hepato-Pancreato-Biliary Surgery and Liver Transplantation Unit,University of Modena and Reggio Emilia,Modena 41121,Italy
Emanuele Felli,Taiga Wakabayashi,Institut de Recherche Contre les Cancers de l'Appareil Digestif(IRCAD),Strasbourg 67000,France
Patrick Pessaux,Service de Chirurgie Viscérale et Digestive,Nouvel H?pital Civil,Strasbourg 67000,France
Tullio Piardi,Department of Surgery,H?pital Robert Debré,Reims 51092,France
Antonio Rampoldi,Interventional Radiology Unit,Niguarda Hospital,Milan 20162,Italy
Renè Adam,Daniel Cherqui,Department of Surgery,Centre Hepatobiliaire,Hopital Paul Brousse,Paris 94000,France
Abstract BACKGROUND The impact of obesity on surgical outcomes in elderly patients candidate for liver surgery is still debated.AIMTo evaluate the impact of high body mass index(BMI)on perioperative and oncological outcome in elderly patients(> 70 years old)treated with laparoscopic liver resection for hepatocellular carcinoma(HCC).METHODS Retrospective multicenter study including 224 elderly patients(> 70 years old)operated by laparoscopy for HCC(196 with a BMI < 30 and 28 with BMI ≥ 30),observed from January 2009 to January 2019.RESULTS After propensity score matching,patients in two groups presented comparable results,in terms of operative time(median range:200 min vs205 min,P= 0.7 respectively in non-obese and obese patients),complications rate(22% vs26%,P= 1.0),length of hospital stay(median range:4.5 d vs 6.0 d,P= 0.1).There are no significant differences in terms of short- and long-term postoperative results.CONCLUSION The present study showed that BMI did not impact perioperative and oncologic outcomes in elderly patients treated by laparoscopic resection for HCC.
Key Words:Hepatocellular carcinoma;Body mass index;Laparoscopy;Surgical resection;Elderly patients;Propensity score matching
lNTRODUCTlON
Obesity is a significant contributing factor for the development of liver disease,starting from the stage of non-alcoholic steatohepatitis up to cirrhosis and hepatocellular carcinoma(HCC)[1-4].Due to the constant increase of population aging,the treatment of HCC in elderly obese patient has become a global clinical issue[5].Laparoscopic liver resection(LLR)provides the benefits of minimally invasive approach in terms of short-term outcomes[6,7],guaranteeing oncological results comparable to the open surgical approach[8,9].However,data about the impact of obesity in patients undergoing LLR remain controversial,with some studies reporting higher body mass index(BMI)as a predictor of an adverse postoperative outcome[10]and other studies not reporting an increased risk of postoperative morbidity linked to obesity[11].The aim of this study was to evaluate the impact of BMI in elderly patients undergoing LLR for HCC,by comparing short- and long-term outcomes.
MATERlALS AND METHODS
This multicenter retrospective study included 224 patients treated between January 2009 and January 2019,at the following centers:Policlinico di Bari,Bari,Italy;Policlinico di Modena,Modena,Italy;Ospedale San Raffaele,Milan,Italy;Grande Ospedale Metropolitano Niguarda,Milan,Italy;Centre hé pato-biliaire Paul Brousse,Villejuif,France;H?pitaux Universitaires Henri Mondor,Créteil,France;Hospital Universitario Sofía,Córdoba,Spain;H?pitaux Universitaires de Genève,Geneva,Switzerland;Nouvel H?pital Civil,Strasbourg,France;Centre Hospitalier Universitaire,Reims,France.
This study investigated patients resected for HCC demonstrating the following inclusion criteria:Child-Pugh class A and B disease;age ≥ 70 years;no evidence of major vessel branch invasion and no distant metastases.Based on the World HealthOrganization(WHO)definition of obesity(BMI > 30 kg/m2)[12]patients were divided in two groups:BMI < 30 kg/m2group and BMI > 30 kg/m2group.
The diagnosis of HCC was done,according to the European Association for Study of Liver(EASL)consensus criteria[13],based on non-invasive findings or histopathology.The type of treatment was planned following multidisciplinary tumor board discussions.
LLR procedure
The surgical procedure was planned based on tumor features and liver function.Minor and major liver resections were performed according Brisbane classification[14].The choice of position and the size of trocars depended by tumor location.Intraoperative ultrasonography represented a standardized initial step of surgical procedure.Liver parenchymal transection was performed with laparoscopic instruments using various energy devices such as the cavitation ultrasonic surgical aspirator ultrasonic,monopolar and bipolar forceps.The extent of resection depended on the size and anatomical location of the tumor and they were defined as “minor” for the resection of two or fewer Couinaud’s liver segments,and ‘major’ for the resection ≥ 3 liver segments.The hepatic hilum was prepared for the Pringle’s maneuver.The specimen was placed in an endocatch bag and removed from one of the trocars’ incision sites.
Follow-up
Short-term outcomes after liver resection included the evaluation of the parameters in the perioperative period,including intraoperative variables such as operative time,and blood transfusion rate,and postoperative variables as complications rate(based on the Clavien-Dindo classification[15]),and length of hospitalization.Long-term outcomes included oncological results in terms of overall survival and disease-free survival(DFS).Liver blood tests were assessed on first,third and fifth postoperative day.Follow-up was performed once every 3 mo during the first year and every 4 mo thereafter with CT-scan and blood tests(including liver function and oncologic markers).Recurrence after treatment included repeat resection,locoregional treatment,till liver transplantation,or supportive care based on the patient’s general status and liver disease according to the EASL-EORTC clinical practice guidelines[13].
Statistical analysis
Statistical analyses were carried out using the IBM SPSS Statistics 20 software.Thet-test and Mann-WhitneyUtest were used to compare continuous variables.The chi-square test and Kruskal-Wallis test respectively was performed to compare categorical variables.The Kaplan-Meier method was used to assess recurrence-free survival(RFS)and overall survival(OS)curves.The Cox proportional hazard model was performed to analyse independent prognostic factors of longterm survival.A propensity score matching(PSM)analysis was performed to reduce selection bias obtaining two more homogeneous matched groups of patients in the resection and ablation groups.Variables included in our propensity model included age,comorbidities ≥ 2,American Society of Anesthesiologists(ASA)score,Child-Pugh and model for end-stage liver disease(MELD)scores,extent of resection,tumor number and size.A one-to-one PSM was performed with a caliper width of < 0.2 of the pooled standard deviation of estimated propensity scores,applying these variables to a logistic regression model and calculated C-statistics.A total of 27 out of the 196 patients in the BMI < 30 group and a total of 27 out of the 28 patients in the BMI > 30 group were matched for further analyses.
RESULTS
Before PSM
We included 224 patients treated with LLR for an HCC and aged ≥ 70 years.One hundred and ninty-six patients presented a BMI < 30 kg/m2and 28 patients presented a BMI > 30 kg/m2.Demographic data were similar between two groups,except for a higher rate of male in BMI ≥ 30 kg/m2group than in BMI < 30 kg/m2group(69%vs93%,P= 0.001).Associated comorbidities were not increased in obese patients,as ASA and MELD score(Table 1).
Perioperative and postoperative data are described in Table 2.There were no significant differences in surgical time(median range:200 minvs220 min,P= 0.70,in the BMI < 30 and BMI > 30 respectively),rate of blood transfusion(16%vs3%,P= 0.09),length of hospitalization(median range:6.0 dvs5.5 d,P= 0.20)
The global rate of postoperative complication was higher in the non-obese group(47%vs25%,P= 0.02)compared to the obese group.Only the rate of wound infection was higher in the obese group(11%vs2%,P= 0.04).
The 90-d mortality rate didn’t present significative difference between the two groups(5% in BMI < 30 group and 0% in BMI > 30 group,P= 0.60).The estimated 1- and 3-year OS rates were 100% and 92.3% in BMI > 30 group,and 96% and 91.4% in BMI < 30 group(P= 0.004;Figure 1A)respectively.The estimated 1- and 3-year DFS rates were 96% and 67% in BMI > 30 group,and 82% and 36% in BMI < 30 group(P= 0.50;Figure 1B)respectively.
After PSM
After matching,we obtained a more homogeneous population for both groups(Table 1).The variables included in the PSM were age,comorbidities,ASA and MELD score,Child Pugh score,tumor size,tumor number and extent of resection.Peri-operative and post-operative results are analytically described in Table 2.The post-operative follow up didn’t reveal any difference in the complication’s rate between BMI > 30 and BMI < 30 group(26%vs22%,P= 1.0),nor in grade of severity(Clavien-Dindo grades III-IV)(4%vs7%P= 0.6).Moreover,operative time(median range:205 minvs200 min,P= 0.7)and rate of blood transfusion(3%vs18%,P= 0.2)were similar.The estimated 1- and 3-year overall survival rates were 100% and 92.3% in the BMI > 30 group,and 88.4% and 83.5% in the BMI < 30 group(P= 0.2;Figure 1C).
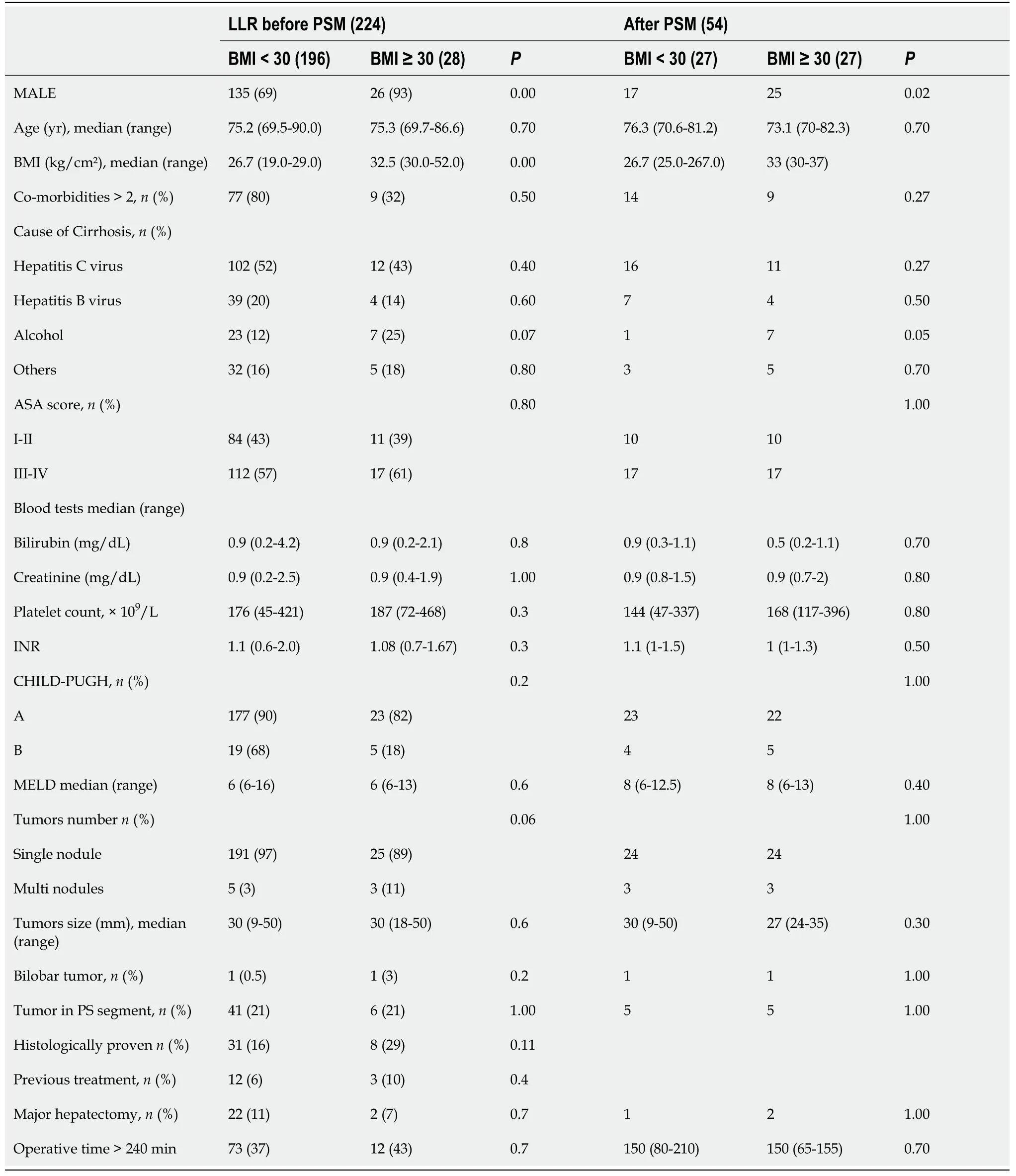
Table 1 Preoperative and clinical characteristics of elderly patients with hepatocellular carcinoma with a body mass index < 30 or ≥ 30 who underwent laparoscopic liver resection
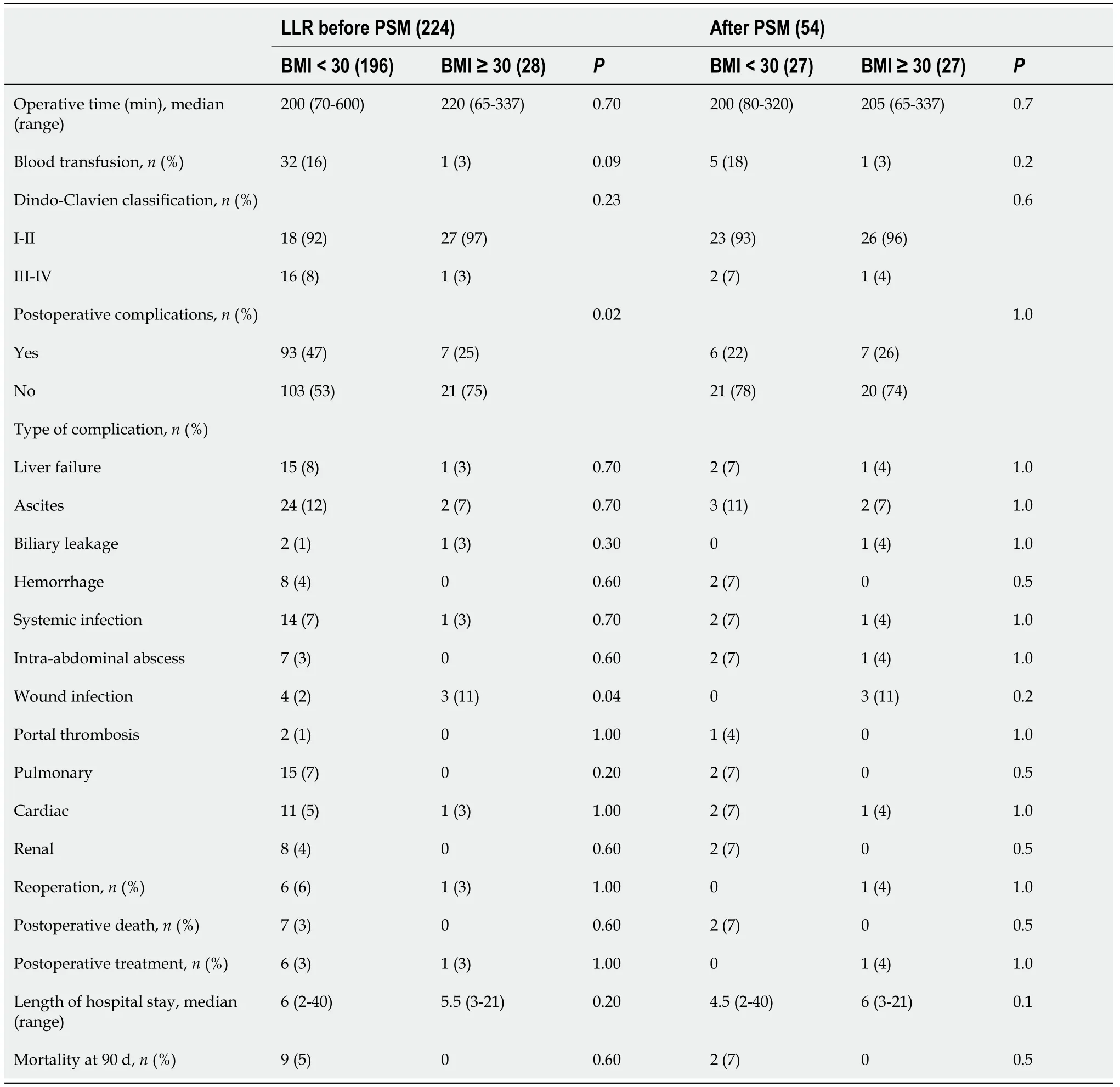
Table 2 Preoperative and clinical characteristics of elderly patients with hepatocellular carcinoma with a 30 > body mass index ≥ 30 who underwent laparoscopic liver resection
The estimated 1- and 3-year DFS rates were 96.2% and 65.8% in the BMI > 30 group,and 87.5% and 86.2% in the BMI < 30 group(P= 0.5;Figure 1D)respectively.
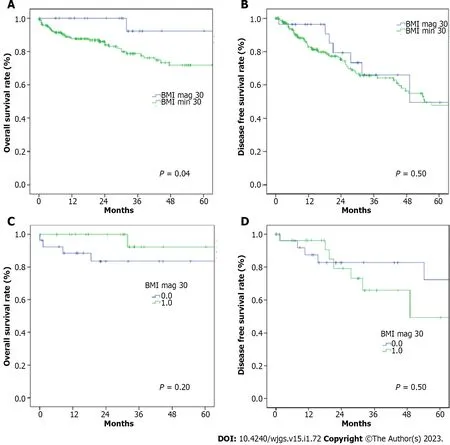
Figure 1 Survival curves and Tumor recurrence curves(Kaplan-Meier method)of elderly patients with hepatocellular carcinoma with a 30 > body mass index ≥ 30 who underwent laparoscopic liver resection before propensity score matching.A:Overall survival(OS)curves were constructed using the Kaplan-Meier method and compared using the log-rank test,OS significantly did not differ between the two groups;B:Recurrence-free survival(RFS)curves were constructed using the Kaplan-Meier method and compared using the log-rank test,hepatocellular carcinoma recurrence significantly differs between the two groups;C:OS curves were constructed using the Kaplan-Meier method and compared using the log-rank test;after propensity score matching,survival remained significantly different;D:RFS curves were constructed using the Kaplan-Meier method and compared using the log-rank test;after propensity score matching,recurrence remained significantly different.BMI:Body mass index.
DlSCUSSlON
The impact of obesity on surgical results in elderly patients who underwent liver resections remains a subject of vivid debate.An increased surgical risk has been expected because of comorbidities,associated to obesity and old age,underlying liver disease and technical difficulties[16-20].Our multicenter study did not confirm this hypothesis and showed that LLR can be safely performed in treatment of HCC also in elderly patients with a BMI ≥ 30 kg/m2.The evaluation of the influence of BMI in elderly population is important because of the increasing prevalence of this condition associated to an higher average life expectancy[21,22].
The increasing BMI has been reported as a predisposition to develop various diseases,including diabetes mellitus,hypertension,respiratory disease and certain type of cancers[23-25].Our data did not show differences in term of rate of comorbidities or tumor characteristics,even after PMS analysis,according to various preoperative parameters(age,comorbidities,ASA and MELD score,Child Pugh score,tumor size,and tumor number and extent of resection),which resulted in a more homogeneous and therefore comparable population.
Even though the initial hypothesis that obesity negatively affected the outcomes of minimally invasive approach was not verified[26],data regarding LLR in obese patients were controversial.After the evaluation of surgical procedures ended with Second International Consensus Conference on LLR[27],a scoring system was built to stratify LLR into groups with increasing degree of difficulty[28].This IWATE score aimed to preoperatively predict,the technical difficulty of various LLR,but without including body habitus.So,the question whether anthropometric variables really have an impact on perioperative outcomes,remains.
Using operative time,rate of blood transfusion and rate of conversion as surrogates of surgical difficulty,Omeet al[29]reported significantly longer median operation time in obese compared to nonobese patients,while for Uchidaet al[30]BMI was an independent predictor of longer operative time > 200 min.Leeet al[31]reported a significant difference in operative time and incidence of blood transfusion in overweight compared to normal weight patients,but no difference for obese patients.In accordance to the abovementioned data,the results of this study also suggest similar rate of blood transfusion and operative time in patients with BMI < 30 kg/m2and those with BMI ≥ 30 kg/m2.
The advantages of a minimally invasive approach in liver surgery,including lower abdominal wall morbidity and early postoperative rehabilitation[32,33],may be more beneficial for the subgroup of obese patients.A recent systematic review[34]reported similar rates of postoperative complications between obese and non-obese patients,although several issues including discrepancy in the obesity definition,limit the validity of these results.Nomiet al[35]reported that the postoperative course of obese patients was not negatively affected by a higher incidence of infectious complications nor liverspecific complications.Yuet al[36]reported a higher rate of bile leak in obese compared to non-obese patients.The herein presented data demonstrate a similar postoperative outcome,with no significant differences in major complications(Clavien Dindo III-IV)nor liver related complications in obese compared to non-obese patients.
View magnification of,optimal exposure with liver mobilization and the increase of dedicated tools allow a clearer visualization of deep structures,small vessels and biliary ducts[7,36,37].The authors speculate this “power” of laparoscopy can justify a lower rate of postoperative complications not only interms of preservation of abdominal wall integrity,linked with prevention on respiratory diseases and reduction of postoperative pain,but also with a greater accuracy in resection technique,especially in the hands of experienced surgeons.
Oncological outcomes following PSM were also similar,as no differences were noted in disease-free and overall survival in obesevsnon-obese patients,undergoing LLR for HCC.This is also in accordance with in the majority of published data[34].These results suggest that also elderly obese patients can benefit from surgical treatment in terms of long-term outcomes,mainly driven by the excellent shortterm outcome of laparoscopy.
CONCLUSlON
In conclusion,according to the present study,BMI does not impact surgical outcomes of LLR in elderly patients treated for HCC.Thorough patient selection,based on liver volume and function evaluation,as well as patient habitus and comorbidities,could result in safe and feasible LLR in elderly obese patients.
ARTlCLE HlGHLlGHTS
Research background
A high body mass index(BMI)could represent a factor which impacts perioperative outcomes in elderly patients who underwent laparoscopic liver resection(LLR).
Research motivation
To evaluate of postoperative outcomes between elderly(age > 70 years)patients with a BMI ≥ 30 and BMI < 30 who underwent a LLR for hepatocellular carcinoma(HCC).
Research objectives
The analysis of short(perioperative)and long-term(oncological results)outcomes.
Research methods
The analysis of data was performed before and after propensity score matching.
Research results
After propensity score matching,patients in two groups presented comparable results,in terms of operative time complications rate length of hospital stay.There are no significant differences in terms of short- and long-term postoperative results.
Research conclusions
The present study showed that BMI did not impact perioperative and oncologic outcomes in elderly patients treated by laparoscopic resection for HCC.
Research perspectives
Randomized controlled studies are needed to better explore these results.
FOOTNOTES
Author contributions:Conticchio M,Inchingolo R,Delvecchio A,Ratti F,Gelli M,Anelli MF,Laurent A,Vitali GC,Magistri P,Assirati G,Felli E,Wakabayashi T,Pessaux P,Piardi T,di Benedetto F,de’Angelis N,Brice?o J,Rampoldi A,Adam R,Cherqui D,Aldrighetti LA,and Memeo R equally contributed to this paper with conception and design of the study,literature review and analysis,drafting and critical revision and editing,and final approval of the final version.
lnstitutional review board statement:This study didn’t require the approval by the Ethics Committee of the Azienda Ospedaliera Universitaria Policlinico of Bari,General Regional Hospital “F.Miulli”,Acquaviva delle Fonti(BA),San Raffaele Hospital of Milan,Gustave Roussy Cancer Campus Grand Paris of Paris,Hospital University Reina Sofía of Córdoba,Centre hospitalier universitaire Henri Mondor of Paris,Geneva University Hospitals and Medical School of Geneva,University of Modena and Reggio Emilia of Modena,Institut de Recherche Contre les Cancers de l’Appareil Digestif(IRCAD)of Strasbourg,H?pital Robert Debré of Reims,Niguarda Hospital of Milan,Centre Hepatobiliaire,Hopital Paul Brousse,of Paris.
lnformed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:All the authors are aware of the content of the manuscript and have no conflict of interest.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORClD number:Maria Conticchio 0000-0003-3177-5274;Riccardo Inchingolo 0000-0002-0253-5936;Antonella Delvecchio 0000-0002-7759-4340;Francesca Ratti 0000-0002-4710-6940;Maximiliano Gelli 0000-0001-9807-4021;Massimiliano Ferdinando Anelli 0000-0002-0916-1949;Alexis Laurent 0000-0003-1372-0843;Giulio Cesare Vitali 0000-0001-8956-0247;Paolo Magistri 0000-0001-8326-069X;Giacomo Assirati 0000-0001-8240-1497;Emanuele Felli 0000-0002-6510-1457;Taiga Wakabayashi 0000-0002-5074-0205;Patrick Pessaux 0000-0001-5635-7437;Tullio Piardi 0000-0001-6704-3206;Fabrizio di Benedetto 0000-0002-6718-8760;Nicola de'Angelis 0000-0002-1211-4916;Javier Brice?o 0000-0001-7027-7898;Antonio Rampoldi 0000-0003-2494-5925;Renè Adam 0000-0003-2169-5449;Daniel Cherqui 0000-0001-5270-2731;Luca Antonio Aldrighetti 0000-0001-7729-2468;Riccardo Memeo 0000-0002-1668-932X.
S-Editor:Chen YL
L-Editor:A
P-Editor:Chen YL
 World Journal of Gastrointestinal Surgery2023年1期
World Journal of Gastrointestinal Surgery2023年1期
- World Journal of Gastrointestinal Surgery的其它文章
- Hereditary polyposis syndromes remain a challenging disease entity:Old dilemmas and new insights
- Application of ablative therapy for intrahepatic recurrent hepatocellular carcinoma following hepatectomy
- Postoperative adjuvant therapy for hepatocellular carcinoma with microvascular invasion
- Prognostic effect of excessive chemotherapy cycles for stage ll and lll gastric cancer patients after D2 + gastrectomy
- Development and validation of a novel nomogram for predicting overall survival in gastric cancer based on inflammatory markers
- New perspectives on robotic pancreaticoduodenectomy:An analysis of the National Cancer Database
