Diagnostic and decision-making difficulties:Placenta accreta at nine weeks’gestation
Achour Radhouane, Bouriel Ines, Neji KhaledEmergency Department of maternity and Neonatology Center, Tunis, Tunisia, Faculty of Medicine of Tunis
ABSTRACT
The majority of cases of placenta accreta are unanticipated and initially identified intraoperatively. Although color Doppler ultrasound is adequate for the evaluation of placenta accreta in the third trimester, ultrasound diagnosis in the first trimester has never been reported. To our knowledge, this is the first case of placenta accreta detected at 9 weeks' gestation by ultrasound. Placenta accreta with intraplacental lacunae can be identified together with a loss of the hypoechogenic retroplacental myometrial zone. Based on this case, we found that early diagnosis of placenta accreta in the first trimester by ultrasound is possible.
ARTICLE INFO
Article history:
Received 22 August 2015
Received in revised form 16 October 2015 Accepted 1 November 2015
Available online 1 January 2016
?
Diagnostic and decision-making difficulties:Placenta accreta at nine weeks’gestation
Achour Radhouane★, Bouriel Ines, Neji Khaled
Emergency Department of maternity and Neonatology Center, Tunis, Tunisia, Faculty of Medicine of Tunis
ABSTRACT
The majority of cases of placenta accreta are unanticipated and initially identified intraoperatively. Although color Doppler ultrasound is adequate for the evaluation of placenta accreta in the third trimester, ultrasound diagnosis in the first trimester has never been reported. To our knowledge, this is the first case of placenta accreta detected at 9 weeks' gestation by ultrasound. Placenta accreta with intraplacental lacunae can be identified together with a loss of the hypoechogenic retroplacental myometrial zone. Based on this case, we found that early diagnosis of placenta accreta in the first trimester by ultrasound is possible.
ARTICLE INFO
Article history:
Received 22 August 2015
Received in revised form 16 October 2015 Accepted 1 November 2015
Available online 1 January 2016
Keywords:
E-mail:Radhouane.A@live.com
1. Introduction
Placenta accreta (PA) is a life-threatening obstetrical condition that occurs when a defect of the decidua basalis enables the direct apposition of chorionic villi to the myometrium. As a result, at least part of the placenta cannot separate after delivery and this may lead to severe obstetric hemorrhage [1]. It has become the principal indication for postpartum hysterectomy as well as for related surgical injuries [2].
The prevalence of accreta is estimated to be 1 in 2 500 pregnancies, but in women with placenta previa the prevalence is 5%-10%[3]. The incidence of PA has increased 4-folds at the last years, following the increase in cesarean delivery rates [4].
It is important to diagnose PA prior to delivery, to allow for optimal concerted management planning and prevention of severe maternal morbidity and mortality [5].
The earliest preoperative diagnosis of placenta increta by ultrasound was at 18 weeks’ gestation [3]. The timing of the defective trophoblast implantation leading to PA suggests that this condition could be identified during the first trimester ultrasound. Signs of PA have been recognized as early as the first trimester in several case reports [6-7]. we report the case in which these abnormal findings were detected at 9 weeks’ gestation in a patient with a poor obstetric history.
2. Case report
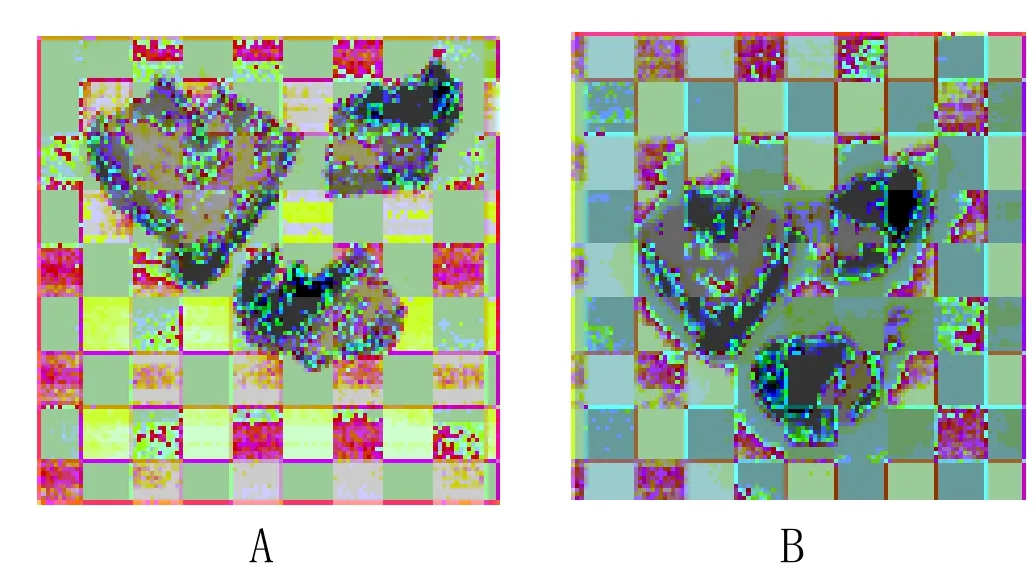
A 35-year-old woman, gravida 4 para 3, she had previously given birth normally to two children and to a third by caesarean section, was referred for vaginal bleeding at 09 + 0 weeks’ gestation. On admission, transvaginal ultrasound revealed an intrauterine pregnancy with a detectable heart beat (Figure 1). The gestational age was estimated by measurement of crown-rump length (25 mm) to be 9 weeks. The placenta was located in the lower ventral portion of the uterus and covered the internal os. Many large and irregularly-shaped lacunae (Grade 3+) were observed and no retroplacental clear zone was seen. Color Doppler ultrasound showed hypervascularity of these dilated lacunar spaces.
The site was well vascularized and there was the suspicion of an invasive mole. The laboratory finds at admission were:haemoglobin12.3g/dL, β-HCG level 140 000UI/mL. Though β-HCG level and the ultrasound examined , an invasive mole could not be excluded. Two days after admission, the evolution has been marked by the spontaneous cessation of pregnancy. Therefore CT scans of the abdomen and pelvis, a chest X- ray of the cranium were performed as part of obligatory staging process. All were normal.
A curettage was indicated and performed under sonographic control after informed consent. Heavy bleeding occurred that could not be managed even after suturing of the uterine arteries; hence an abdominal hysterectomy had to be performed (blood loss 1 400 mL). Six units of packed red blood cells were transfused. The patient was discharged without any complications 5 days post-operation.
The uterus was (14×10×6) cm. Histological examination of the surgical specimen confirmed the diagnosis of placenta accreta (Figure 2). Pathological anatomic examination revealed chorionic villi extending beyond the confines of the endometrium and attaching to the superficial aspect of the myometrium and cervix. There was no evidence for a hydatiform mole or a chorionepithelioma.
Figures 2. Histological section confirming placenta accreta.
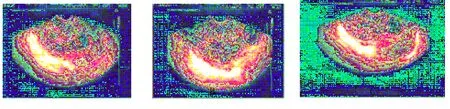
Figure 1. Transvaginal fetal ultrasound at 9 weeks’ gestation.Note the absence of the hypoechogenic retroplacental complex. There are prominent hypoechogenic-anechogenic spaces (lacunae) in the placenta.
3. Discussion
PA is a life-threatening obstetrical emergency. Its incidence has risen in parallel with that of cesarean deliveries and it remains a major cause of maternal mortality and morbidity as the principal indication for post partum hysterectomy [5-8]. Efforts have been made to refine the ultrasound diagnosis of PA in the first trimester of pregnancy.
During the first trimester, on reviewing medical literatures over the past 20 years, the reported cases of PA (6-12 weeks) were mostly discovered after the occurrence of severe bleeding either during the abortive curettage [9-10] or in the post abortive weeks [11-12]. Thus the case described here represents a very rare case situation.
However, In the first trimester PA, it is likely to develop at the time of the trophoblast invasion [13]. The study of the trophoblast’s location in the first trimester is feasible and must be considered as part of routine scan. The sonographic diagnosis of PA has been reported in few cases [6] in the first trimester as a low gestational sac, suggesting a direct implantation of the trophoblast over the scar, essentially a low-lying gestational sac and diffuse dilatation of the intra-placental vessels called lacunae[6]. Additionally, PA could be suspected if a part of the lining of the gestational sac was embedded in the previous Cesarean section scar with an irregular decidual layer and thinning of the underlying uterine wall [6].
The main reported cases are the following:The earliest reported detection of a low-lying gestational sac, known retrospectively to be associated with PA, was at 5 and 6 weeks’ gestation.The sac was discovered near the internal os and a diagnosis of Cesarean scar pregnancy was made. This suggested a direct implantation of the trophoblast over the scar. After follow up, cesarean section and subtotal hysterectomy were performed with the final diagnosis of anterior placenta previa/accreta [14]. However, these cases are difficult to differentiate from ectopic pregnancies developing in the LSCS (low sac cesarean section) scar [15].
Similar retrospective studies reported prenatal diagnosis of 8 cases of PA, after previous cesarean deliveries, in which ultrasound examination was performed between 8-10 weeks’ gestation. These cases all showed gestational sac located in the lower uterine segment at the site of the Cesarean section scar and were allproven to have PA by histopathological examination [16]. Using this ultrasonographic finding Chen et al. reported transvaginal sonographic diagnosis of PA as early as 8 and 9 weeks’ gestation. They also had to perform hysterectomy owing to heavy bleeding, either immediately or few weeks later, with histopathological confirmation of PA [6]. In the present case, massive vaginal bleeding and hypovolemic shock occurred during termination; in order to save her life, an emergency hysterectomy was performed, although preservation of fertility was attempted[3].
Recently, Stirnemann et al. [13] implemented these first trimester signs of placenta PA in a prospective screening trial. They suggested that the rationale for 11-14 weeks’ screening in the high-risk group allowed early diagnosis and planning for optimal management.
Similarly, the placenta accreta may be biologically detected:Deirrdre et al, demontrate, among women with placenta previa, a strong increased risk for placenta accreta with elevated first trimester PAPP-A and a strong decreased risk when IPI (Interval Inter Pregnancies) was prolonged (more than 60 months). These novel associations may inform the diagnosis and mechanism of placenta accreta and warrant further investigation [17].
Early ultrasound evaluation during the first trimester is recommended for patients who are at risk of invasive placentation. Based on this case, we found that early diagnosis of placenta accreta in the first trimester is possible [3].
The differential diagnoses, for example, an invasive mole, should not be neglected. Early diagnosis may allow earlier elective intervention that prevents maternal morbidity and mortality.
Declare of interest statement
We declare that we have no conflict of interest.
References
[1] Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol 2006;107:1226-1232.
[2] Shellhaas CS, Gilbert S, Landon MB, Vamer MW, Leveno KJ, Hauth JC, et al. The frequency and complication rates of hysterectomy accompanying cesarean delivery. Obstet Gynecol 2009;114:224-229.
[3] Chen YJ, Wang PH, Liu WM, Lai CR. Placenta accreta diagnosed at 9 weeks’ gestation. Ultrasound Obstet Gynecol 2002; 19:620-622.
[4] Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation:twentyyear analysis. Am J Obstet Gynecol 2005;192:1458-1461.
[5] Briery CM, Rose CH, Hudson WT, Lutgendorf MA, Magann EF, Chauhan SP, et al. Planned vs emergent cesarean hysterectomy. Am J Obstet Gynecol 2007;197:154.e1-5.
[6] Shih JC, Cheng WF, Shyu MK, Lee CN, Hsieh FJ. Power Doppler evidence of placenta accreta appearing in the first trimester. Ultrasound Obstet Gynecol 2002;19:623-625.
[7] Comstock CH, Lee W, Vettraino IM, Bronsteen RA. The early sonographic appearance of placenta accreta. J Ultrasound Med 2003;22:19-26.
[8] Eller AG, Bennett MA, Sharshiner M, Masheter C, Soisson AP, Dodson M, et al. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet Gynecol 2011;117:331-337.
[9] Yang JI, Kim HY, Kim HS, Ryu HS. Diagnosis in the first trimester of placenta accreta with previous cesarean section. Ultrasound Obstet Gynecol 2009;34:116-118.
[10] Kim K, Pietrzak A, Gonzalez S, Podgony K. Severe hemorrhage in a first-trimester cesarean scar pregnancy during dilation and curettage. Int J Obstet Anesth 2010;19(3):348-349.
[11] Son G, Kwon J, Cho H, Kim Sangwun, Yoon Bosung, Nam Eunji, et al. A case of placenta increta presenting as delayed post abortal intraperitoneal bleeding in the first trimester. J Korean Med Sci 2007; 22(5):932-935.
[12] Wang YL, Su TH, Huang WC, Weng SS. Laparoscopic management of placenta increta after late first-trimester dilation and evacuation manifesting as an unusual uterine mass. J Minim Invasive Gynecol 2011;18(2):250-253.
[13] Pijnenborg R, Dixon G, Robertson WB, Brosens I. Trophoblastic invasion of human decidua from 8 to 18 weeks of pregnancy. Placenta 1980;1:3-19.
[14] Wong HS, Zuccollo J, Parker S, Burns K, Tait J, Pringle KC. Antenatal diagnosis of non-previa placenta increta with histological confirmation. Ultrasound Obstet Gynecol 2006;27(4):467-469.
[15] Stirnemann JJ, Mousty E, Chalouhi G, Salomon LJ, Bernard JP, Ville Y. Screening for placenta accreta at 11-14 weeks of gestation. Am J Obstet Gynecol 2011;205:547.e1-6.
[16] Wong HS, Zuccollo J, Tait J, Pringle KC. Placenta accreta in the first trimester of pregnancy:sonographic findings. J Clin Ultrasound 2009;37(2):100-103.
[17] Deirdre L, Allison F, Rebecca B, Yair B, Maurice D, Yasser S, et al. Placental accreta and first and second trimester maternal serum markers and characteristics. Am J Obstet Gynecol 2014; 2010 (Supplement 1) :S62.
Placenta accrete
Nine weeks' gestation
Ultrasound diagnosis
doi:Document heading 10.1016/j.apjr.2015.12.016
*Corresponding author:Achour Radhouane, Emergency Department of maternity and Neonatology Center, Tunis, Tunisia, Faculty of Medicine of Tunis.
 Asian Pacific Journal of Reproduction2016年1期
Asian Pacific Journal of Reproduction2016年1期
- Asian Pacific Journal of Reproduction的其它文章
- Male masturbation device for the treatment of premature ejaculation
- Risk factors and adverse perinatal outcomes associated with low birth weight in Northern Tanzania:A registry-based retrospective cohort study
- Analysis of the androgen receptor CAG repeats length in Iranian patients with idiopathic non-obstructive azoospermia
- Returning of cyclicity in infertile Corriedale Sheep with natural progesterone and GnRH based strategies
- Effect of cooling to different sub-zero temperatures on boar sperm cryosurvival
- Milk supplements in a glycerol free trehalose freezing extender enhanced cryosurvival of boar spermatozoa
