Ambulatory diastolic blood pressure: a marker of comorbidity in elderly fit hypertensive individuals?
Alfredo De Giorgi, Rosaria Cappadona, Caterina Savriè, Benedetta Boari, Ruana Tiseo,Giulia Marta Viglione, Christian Molino, Elisa Misurati, Mauro Pasin,, Roberto Manfredini,,Fabio Fabbian,,?
1. Clinica Medica Unit, Azienda Ospedaliero-Universitaria S. Anna, Ferrara, Italy; 2. Department of Medical Sciences,University of Ferrara, Ferrara, Italy
ABSTRACT BACKGROUND Masked diastolic hypotension is a new blood pressure (BP) pattern detected by ambulatory blood pressure monitoring (ABPM) in elderly hypertensives. The aim of this study was to relate ABPM and comorbidity in a cohort of fit elderly subjects attending an outpatient hypertension clinic. METHODS Comorbidity was assessed by Charlson comorbidity index (CCI) and CHA2DS2VASc score. All subjects evaluated with ABPM were aged ≥ 65 years. CCI and CHA2DS2VASc score were calculated. Diastolic hypotension was defined as mean ambulatory diastolic BP < 65 mmHg and logistic regression analysis was carried out in order to detect and independent relationship between comorbidity burden and night-time diastolic BP < 65 mmHg. RESULTS We studied 174 hypertensive elderly patients aged 72.1 ± 5.2 years, men were 93 (53.4%). Mean CCI was 0.91 ± 1.14 and mean CHA2DS2VASc score of 2.68 ± 1.22. Subjects with night-time mean diastolic values < 65 mmHg were higher in females[54.7% vs. 45.3%, P = 0.048; odds ratio (OR) = 1.914, 95% CI: 1.047?3.500]. Logistic regression analysis showed that only CHA2DS2-VASc score was independently associated with night-time mean diastolic values < 65 mmHg (OR = 1.518, 95% CI: 1.161?1.985; P =0.002), but CCI was not. CONCLUSIONS ABPM and comorbidity evaluation appear associated in elderly fit subjects with masked hypotension. Comorbid women appear to have higher risk for low ambulatory BP.
The global population is ageing, and the number of subjects with long-term disorders is increasing, with heavy consequences on medical commitment and health-care systems burden.[1]Moreover, multimorbidity is associated with a higher mortality,[2,3]and hypertension represents a frequent condition involving patients with multiple diseases.[1]The relationship between multimorbidity and hypertension is bidirectional. Hypertension could cause organ damage and then development of comorbidity; on the other hand, comorbidity could worsen hypertension and its consequences. In elderly subjects, hypertension could cause brain damage that could be the cause of cognitive decline;[4]moreover, systemic atheroembolic syndrome could worsen blood pressure (BP) variability leading to cardiovascular disease (CVD).[5]
Hypertension, both complicated or not complicated, is a variable taken into consideration in a series of risk scores applied to the general population to estimate the mortality risk, such as the Cumulative Illness Rating Scale,[6]the Charlson comorbidity index(CCI),[7]and the Elixhauser index.[8]The CHA2DS2VASc score is widely used as predictor of the risk of stroke in patients with atrial fibrillation, it includes hypertension among the factors considered for score calculation and its importance is underlined by the same weight assigned to congestive heart failure (CHF),age > 75 years, and diabetes mellitus (1 point).[9]However, CHA2DS2VASc score has also been suggested to be able to stratify adverse clinical events in hypertensive patients.[10]
In patients with comorbidities, out-of-office monitoring of BP has been shown to be associated with reduced systolic BP (SBP) compared to usual care, representing a very useful tool in routine clinical practice.[11]However, the discrepancy of measures between office and out-of-office BP measures, such as ambulatory blood pressure monitoring (ABPM), is known since two decades,[12]and these two approaches have pros and cons depending also on type of patients. In untreated older patients with isolated systolic hypertension, for example, ambulatory SBP was a significant predictor of cardiovascular risk over and above conventional BP.[13,14]
It is widely accepted that ABPM is a crucial informative tool for the evaluation of BP behaviour in everyday clinical practice,[15]and is recommended to identify white-coat hypertension and masked hypertension.[15,16]However, its importance goes greatly beyond due to its capacity to provide information for clinical use.[15]In fact, night-time evaluation of BP is crucial to detect abnormal patterns of nighttime behaviour, such as non-dipping, inverse dipping, extreme dipping and the morning surge,[17]and asleep SBP is a significant BP derived risk factor for CVD events.[18,19]
Recently, a novel BP pattern defined masked diastolic hypotension, frequently found in older patients under antihypertensive treatment, has raised attention.[20]Knowledge related to clinical use of ABPM in elderly subjects is still a matter of debate,and information about BP components and circadian profiles in subjects with high comorbidity burden is scarce.[21]
The aim of this study was investigate the possible relationship between the BP components (recorded by ABPM) and the comorbidity burden (assessed by means of CCI and CHA2DS2VASc score) in a cohort of fit elderly subjects attending an outpatient hypertension clinic.
METHODS
Study Population and Data Source
This retrospective cohort study analyzed the database of the ABPM recordings of the Hypertension Center of the St. Anna University Hospital of Ferrara,Italy, in the years 2018. It was conducted in agreement with the declaration of Helsinki of 1975, revised in 2013. In order to maintain data anonymity and confidentiality, patient identifiers were cancelled before data analysis, deleting the possibility of identification of subjects, either in this paper or in the database. Analysis of data was part of the usual care protocols of the hypertension clinic, and the Local Ethics Committee approved this study (ABPMCOMELY Study: 757/2021/Oss/AOUFe).
ABPM recordings and clinical data recorded in the hospital database of all subjects aged ≥ 65 years attending the outpatient clinic were considered for analysis. The diagnosis of hypertension was made by general practitioners based on the Italian Society of Hypertension guidelines,[22]and patients were referred to the hypertension clinic of the hospital in order to perform ABPM. The Italian Society of Hypertension adopts the recommendations of the last version of the European Society of Hypertension/European Society of Cardiology.[16]Reason for performing ABPM were: suspected white-coat hypertension, suspected masked hypertension, resistant hypertension, assessment of dipper status, and assessment of treatment efficacy. Data inclusion criteria: elderly fit patients were able to walk as usual during a 24-hour ABPM examination. Data exclusion criteria: dependent frail subjects or patients with cognitive decline, ABPM recordings reporting fewer than 70% of successful SBP/diastolic BP (DBP)readings over a 24-hour duration, or those missing values during two consecutive hours.[23]
ABPM Protocol
ABPM was performed using a portable BP oscillometric device (Model 90207; Space-Labs Medical Inc., Redmond, Washington, USA). Antihypertensive treatment was not discontinued, and all participants were allowed to walk as usual and were required to go to sleep at 23:00. Patients were instructed to maintain their usual activities and to hold the arm still by the side during the BP measurements. The ABPM cuff was placed on the non-dominant arm, and measurements were programmed at 20 min intervals during daytime periods (06:00?23:00) and at 30 min intervals during night-time periods (23:00?06:00). Therefore, we defined 23:00 as the time point to separate the daytime and night-time periods and 06:00 as the time-point to separate night-time and daytime periods. Mean SBP, DBP, pulse pressure and heart rate were calculated.[23]
Office and Home BP Measurement
Office BP was recorded according to the recommendations of the 2018 European Society of Hypertension/European Society of Cardiology guidelines.[16]Three to five BP measurements were carried out in the sitting position after 5-min resting period with a validated automatic oscillometric device, choosing a cuff based on arm circumference. The reported value was the average of the measurements. During clinic evaluation, patients were asked to report the mean values of BP recorded at home.
CCI Calculation
The CCI[7]was conceived in 1987 for predicting mortality rates of patients admitted to the general internal medicine service. This wide used score is capable to predict survival in patients with multiple comorbidities. In fact, each condition has different weights, and the sum of the single scores associated with the presence of a disease, is representative of a measure of total comorbidity burden. Overall, several diseases are included, i.e., myocardial infarction, CHF, peripheral vascular disease, cerebrovascular disease, dementia, chronic obstructive pulmonary disease, connective tissue disease, peptic ulcer disease, liver disease, diabetes mellitus, hemiplegia, moderate to severe chronic kidney disease, solid tumor, leukemia, lymphoma, and acquired immune deficiency syndrome.
CHA2DS2VASc Score Calculation
The CHA2DS2VASc score[9]was suggested to have prognostic values in hypertensive individuals.[10]In order to calculate CHA2DS2VASc score, the following parameters were considered: age between 65 years and 74 years, female sex, hypertension, diabetes mellitus, CHF, and vascular disease (1 point each); and age ≥ 75 years, and history of cerebrovascular accidents (2 points each).
Statistical Analysis
Qualitative data were expressed as counts (percentages) and quantitative variables were expressed as mean ± SD. Data were compared stratifying patients on the basis of comorbidity burden. Results derived from CCI calculation defined three groups:subjects belonging to group 1 had CCI = 0, those belonging to group 2 had CCI = 1 and those belonging to group 3 had CCI ≥ 2. Comorbidity burden calculated by CHA2DS2VASc score classified participants in those with CHA2DS2VASc score = 1 and those with CHA2DS2VASc score ≥ 2. The analysis of variance and Student’st-test were applied as appropriate. Diastolic hypotension was arbitrarily defined as mean ambulatory DBP < 65 mmHg during 24-hour,daytime and night-time periods. Prevalence of diastolic hypotension in the different periods of ABPM and in male and female subjects was calculated. Logistic regression analysis was carried out in order to detect and independent relationship between comorbidity burden and night-time DBP < 65 mmHg,determining the odds ratio (OR) with 95% confidence interval (CI). In the model, night-time DBP <65 mmHg was the dependent variable; while age, CCI,CHA2DS2VASc score and the single clinical conditions taken into consideration were the independent ones. Two-sidedP-value < 0.05 were considered statistically significant. Statistical analysis was performed using IBM SPSS statistics (for windows), version 26.0.
RESULTS
Overall, along the study period recordings by 174 hypertensive elderly fit patients were considered(93 men and 81 women). Clinical characteristics of the population are reported in Table 1, whilst BP values of the patients are shown in Table 2.
As for the CCI, 88 patients had CCI = 0, 41 patients had CCI = 1, 22 patients had CCI = 2, 19 patients had CCI = 3, 3 patients had CCI = 4 and 5 patients had CCI = 5; therefore, 88 patients belonged to group 1 (CCI = 0), 41 patients belonged to group 2 (CCI = 1) and 45 patients belonged to group 3 (CCI ≥2). CHA2DS2VASc score = 1 was calculated in 30 patients and CHA2DS2VASc score ≥ 2 was calculated in 144 patients. BP values stratified according to different values of comorbidity indexes are reported in Tables 3 & 4.
Patients with higher comorbidity burden, were older, the percentage of patients treated with more than three antihypertensive medications was lower and had lower mean diastolic values detected by ABPM;however, comorbidity burden was associated with lower mean systolic night-time values in the case of CCI and higher mean pulse pressure values during 24-hour in the case of CHA2DS2VASc score.
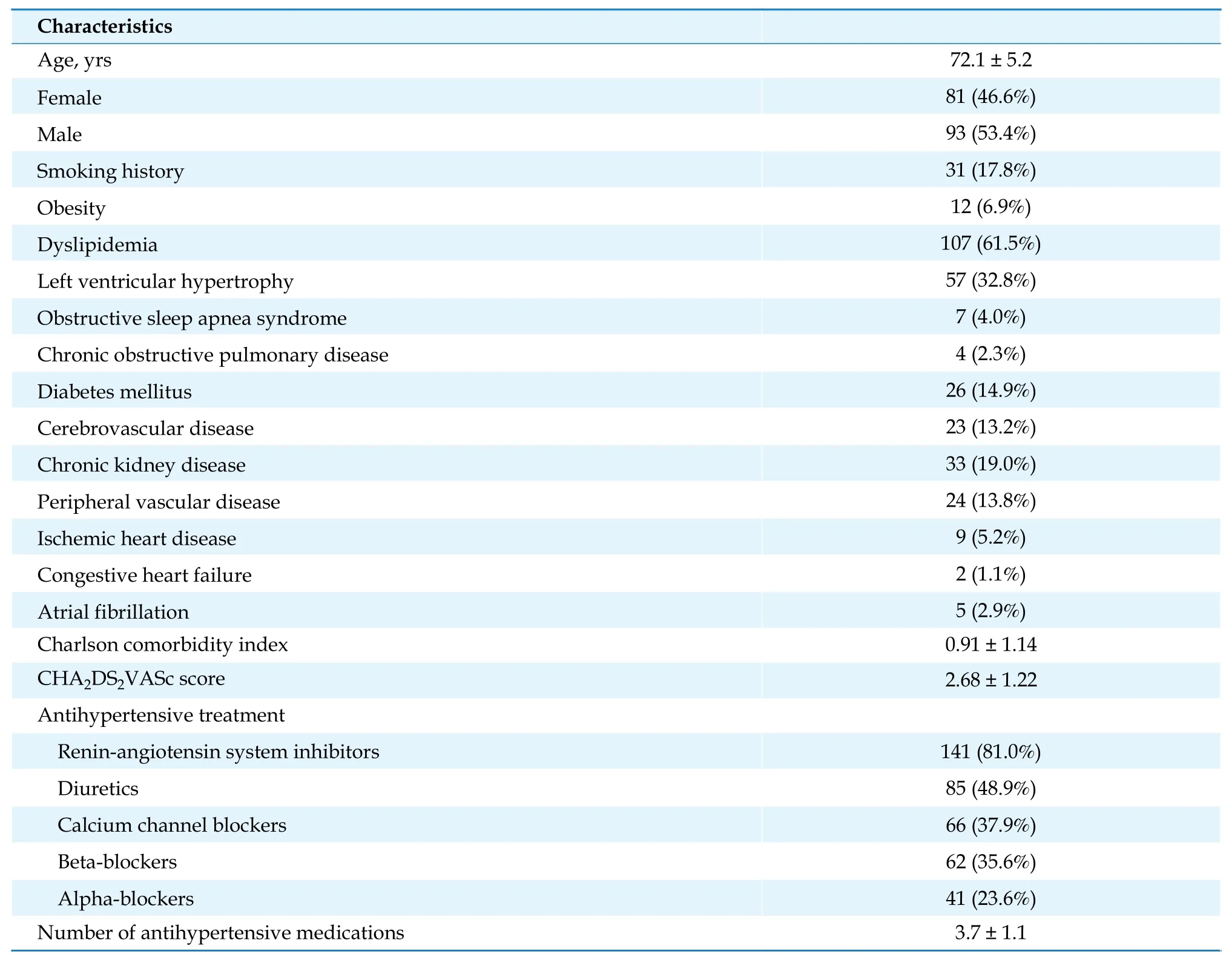
Table 1 Clinical characteristics of the considered population (n = 174).
Diastolic hypotension, defined as mean DBP < 65 mmHg, was detected in 30 subjects (17.2%) along the entire 24-hour period (60.3 ± 3.5 mmHg), in 22 subjects (12.6%) considering daytime only (60.9 ±3.6 mmHg) and in 86 subjects (49.4%) considering night-time only (58.5 ± 4.3 mmHg). Subjects with night-time mean diastolic values < 65 mmHg were higher in females (54.7%vs.45.3%,P= 0.048; OR =1.914, 95% CI: 1.047-3.500). Logistic regression analysis showed that only CHA2DS2VASc score was independently associated with night-time mean diastolic values < 65 mmHg (OR = 1.518, 95% CI: 1.161-1.985;P= 0.002), but CCI was not.
DISCUSSION
The main result of this study, retrospectively analyzing the ABPM recordings of a selected cohort of elderly fit hypertensive subjects, is that comorbidity burden seems to be related with ambulatory DBP. In particular, in older patients with CCI and CHA2DS2-VASc score ≥ 2, the mean ambulatory DBP was lower during 24-hour, daytime and night-time. Moreover, CCI ≥ 2 was also related with low mean ambulatory SBP during night-time, while CHA2DS2VASc score ≥ 2 was related with 24-hour mean pulse pressure. Finally, only CHA2DS2VASc score ≥ 2 was independently associated with mean night-time ambulatory DBP < 65 mmHg. These results are in agreement with recent findings by Kleipoo,et al.,[20]who retrospectively evaluated 848 patients aged 60 years undergoing ABPM. The authors found that ambulatory DBP hypotension, defined as DBP ≤ 70 mmHg,was detected in 22% of the population, and this group of patients showed higher age and comorbidity burden.[20]However, the mean age of patients with DBP hypotension was lower than the mean age of subjects enrolled in our study, being 65 ± 13 years,although the mean CCI was higher. On the other hand, we analyzed data in a different (and opposite)way, starting from stratification of individuals on the basis of their comorbidity burden.
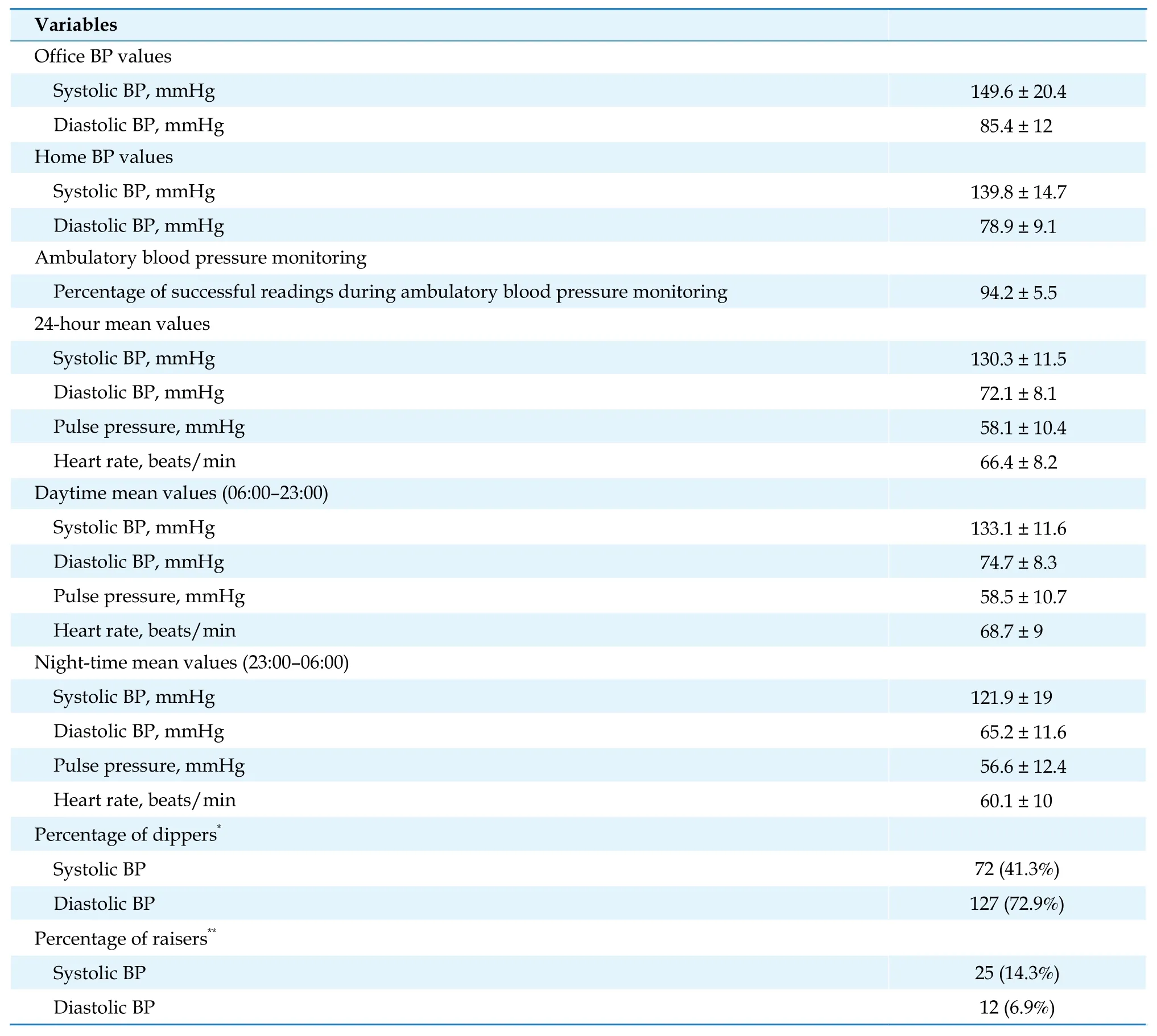
Table 2 Mean values of BP measurements in the considered population (n = 174).
The interpretation of DBP in the elderly is matter of debate. The results from the large cohort of more than 27,000 subjects belonging to the India ABPM study, found a steeper rise in night-time BP with age.[24]
Diastolic hypotension leading to widening pulse pressure suggests different interpretation, pulse pressure could be a clinical marker of arterial stiffening and hypotension could be a common finding in older adults. Arterial aging evaluated by carotidfemoral pulse wave velocity was associated with cognitive function;[25]on the other hand, low pulse wave velocity was associated with young biological vascular age in subjects aged 50-64 years.[26]Although white-coat hypertension and masked hypertension detected by ABPM were associated with early arterial aging,[27]SBP hypotension was reported to be a common finding in elderly patients investigated with ABPM.[28]Subjects investigated by Scuteri,et al.[28]were aged 78.7 ± 7.1 years, a value similar to the mean age of subjects with high comorbidity burden enrolled in our study. It cannot be excluded that hypotensive episodes could be the cause of the relationship between comorbidity burden and lower prevalence of subjects treated with more than three antihypertensive medications, as shown in our study.
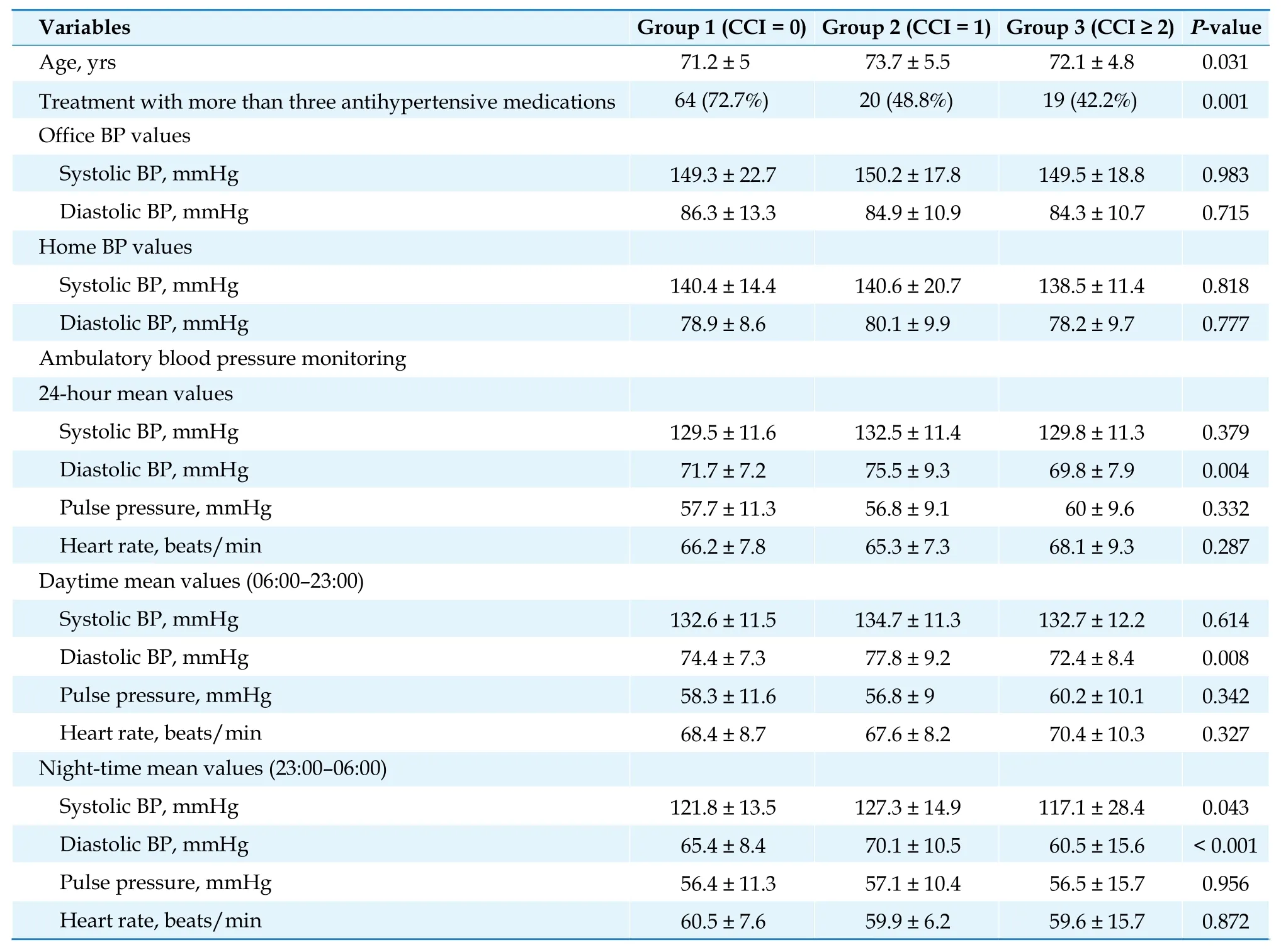
Table 3 Mean values of BP measurements in the three groups stratified by CCI score.
It is known that lowering DBP could lead to development of complications.[29,30]Syncope, hypotension, falls, acute kidney injury with electrolyte abnormalities, and cardiovascular complications have been related to DBP with a J-shaped curve.[30-35]A Jshape relationship between cardiovascular events and BP suggests caution with excessive lowering of diastolic pressure, for example, in individuals with coronary artery disease.[36]On the other hand, the proposed J-shaped relationship between achieved BP level and CVD risk, has been reported only on the basis of clinic BP values, whilst data obtained by ABPM-determined BP are still a matter of debate. In older subjects, difference between office BP and ABPM is significant, and this clinical finding could increase the risk of overtreatment.[37]In fact, the J-shaped curve could be the clinical manifestation of the overtreatment of high BP. Therefore, it was recommended the application of ABPM for the appropriate assessment of awake BP and asleep BP control, in order to better characterize BP profile and time treatment for improving cost-effectively cardiovascular outcome.[38]Moreover, in older patients with hypertension, low ambulatory DBP has been associated with higher risk of death.[39]The 2018 European Society of Hypertension/European Society of Cardiology guideline recommends to avoid to lower DBP < 70 mmHg,especially in subjects with hypertension associated with diabetes mellitus and coronary artery disease.[16]
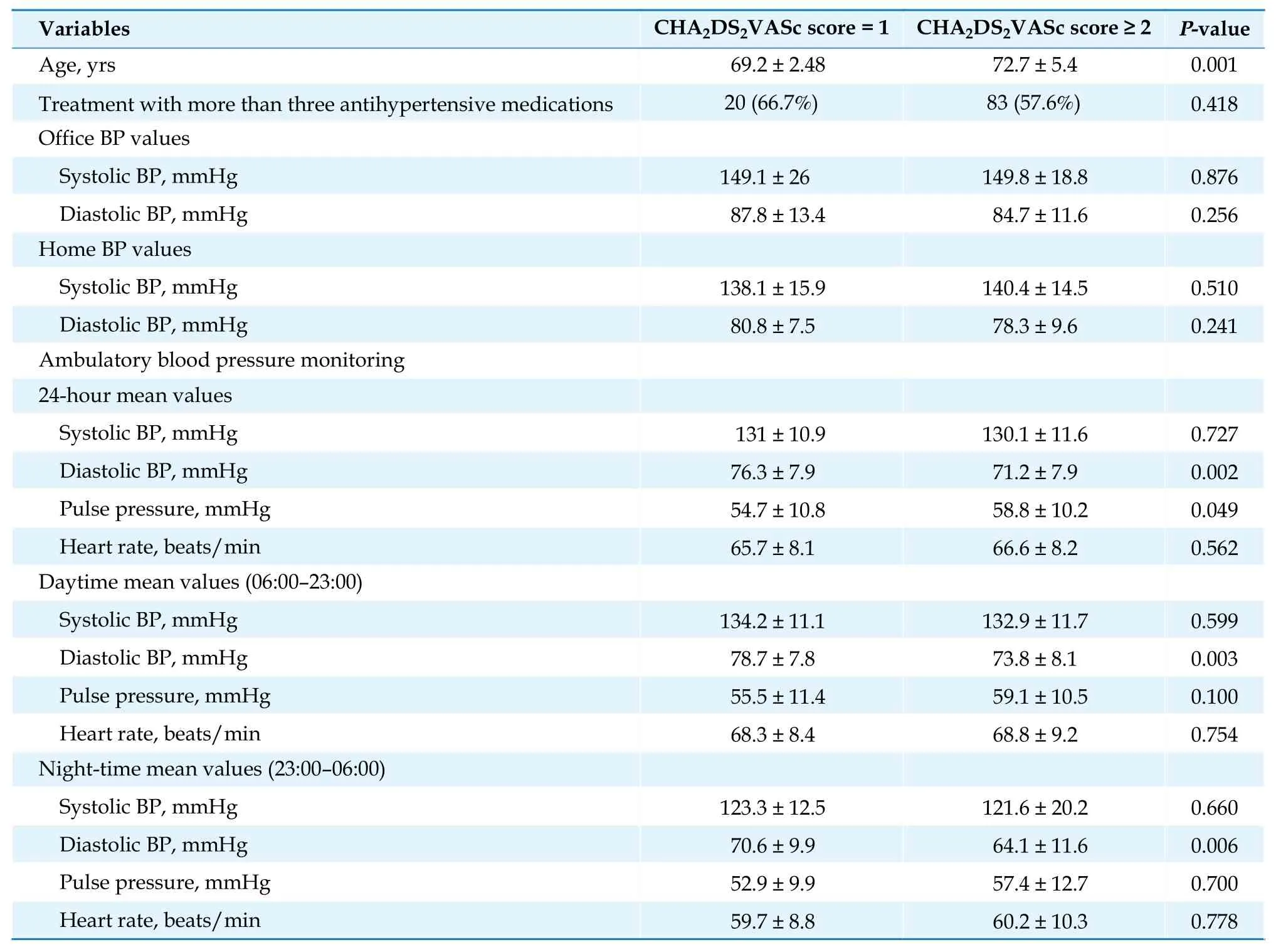
Table 4 Mean values of BP measurements in the two groups stratified by CHA2DS2VASc score.
Individuals aged ≥ 65 years have a higher prevalence of diseases and conditions capable to affect arterial stiffness; moreover, they can demonstrate wide variability of BP with periods of hypotension interspersed with hypertension on ABPM. In this group of patients, ABPM shows increasing 24-hour SBP and mild decreasing 24-hour DBP after 60-70 years of age, leading to increasing 24-hour pulse pressure and the prevalence of 24-hour isolated systolic hypertension. Besides, there is blunted diurnal BP variation (nondipping) and postural and postprandial hypotension. In the elderly, the physiological nocturnal BP fall gradually diminishes with increasing age, and subjects nondippers and risers with higher nocturnal than daytime BP are frequently detected.It has been reported that ABPM should be indicated in persons likely to have a blunted night-time BP decline and elevated CVD risk, such as those with comorbidity.[38,40]The association between CHA2DS2VASc score ≥ 2 and 24-hour mean pulse pressure could be ascribed to increasing arterial stiffness, in elderly patients with low DBP, an increased frequency of cardiovascular events was associated with aortic stiffening and premature wave reflections.[41]
ABPM could be useful in identifying hypotension,a frequent finding in the elderly with autonomic or baroreceptor failure, compromised arterial circulation due to coronary and cerebrovascular disease and frailty.[42]In 2016, Divisón-Garrote,et al.[43]reported that age, female sex, history of ischemic heart disease, and body mass index < 30 kg/m2were independently associated with hypotension in more than 70,000 hypertensives aged 62 years. The same research group evaluated more than 5000 patients aged ≥ 80 years with hypertension enrolled in the Spanish ABPM registry, and showed that 22.8% subjects had office hypotension, 33.7% had daytime hypotension, 9.2% had night-time hypotension, and 20.5%had 24-hour ABPM hypotension. The variables independently associated with office and ABPM hypotension were diabetes mellitus, coronary heart disease, and polytherapy.[44]However, different findings should be taken into account. It has been reported that variability of daytime SBP is a powerful predictor of cardiovascular morbidity in elderly men,independently of other established cardiovascular risk factors suggesting that 24-hour ABPM may contribute to an improved risk assessment in elderly subjects.[45]On the other hand, each 5% rise in nighttime SBP relatively to daytime SBP increases cardiovascular risk by 20%,[46]and the risk for cardiovascular mortality expressed as the hazard ratio for each 5-mmHg rise night-time diastolic pressure was 1.09 (95% CI: 1.04-1.14,P< 0.001).[47]
In addition to the risk of cardiovascular mortality,also the relationship between ABPM data and cerebrovascular disease is still uncertain. On one hand,in elderly subjects, hypertension and in particular the morning surge in BP, are considered predictors of subsequent stroke,[48]and even in normotensives could represent a risk factor for cardiovascular events.[49]On the other hand, nocturnal hypotension and brain hypoperfusion might play a role as well. Kario,et al.[50]reported that in elderly subjects, extreme BP dipping was related to silent and clinical cerebral ischemia through hypoperfusion during sleep or an exaggerated morning rise of BP, while reverse dipping could increase the risk for intracranial hemorrhage.A J-shaped relationship between nocturnal BP and silent cerebral infarcts and stroke incidence during follow-up has been reported, and extreme-dippers and risers showed a higher prevalence of silent cerebral infarcts and a poorer stroke prognosis.[51]Moreover, in elderly subjects with hypertension, ambulatory SBP values and nocturnal systolic dipping were associated with brain matter volume and cognitive function.[52]In elderly men, extreme nocturnal DBP fall could cause focal changes in cerebral blood flow[53]and high ambulatory BP variability in people aged ≥80 years was related to cognitive dysfunction.[54]Similar results were further reported in a population with a mean age of 78 ± 8 years with well-controlled ambulatory BP.[55]Again, in heart failure patients, brain white matter hyperintensities volume and percentage of white matter hyperintensities/total brain volume was higher in the non-dipper group than the dipper group.[56]
LIMITATIONS
This study has several limitations. Firstly, the retrospective design, being an analysis of ABPM recordings of a selected sample of subjects. Secondly, data are single-center collected; therefore, results could not be generalizable. Thirdly, we used CCI, a score that does not allow to quantifies correctly the burden of disease in elderly patients, such as Cumulative Illness Rating Scale.[6]Fourthly, nocturnal period was defined as a fixed night-time period from 23:00 to 06:00, and it is known that different definitions of the night-time yielded significant differences in determining nondipping, extreme dipping and dipping BP patterns. In fact, actigraphy-based approach has been suggested as the best strategy to avoid misclassifications.[57]Reproducibility of nocturnal BP patterns could be modest; therefore, it is necessary to be cautious in drawing conclusions.[58]Last but not least, we evaluated only patients that were under antihypertensive treatment, and we did not evaluate the timing of treatment.
CONCLUSIONS
The 2017 High Blood Pressure Clinical Practice guideline suggests that intensity treatment aiming at BP lowering should be evaluated on the basis of risk/benefit assessment if adults are aged ≥ 65 years and have high comorbidity burden.[15]In elderly population, detection of masked hypotension could be as important as diagnosis of orthostatic BP changes.[59,60]Office BP measurements are usually collected during a narrow interval of time, with the potential risk of inaccuracy and poor correlation with hemodynamic status of patients. ABPM and comorbidity burden evaluation appear effective in diagnosing masked hypotension in fit elderly patients, allowing personalization of antihypertensive treatment. Moreover, sex-specific differences should be taken into account, since our study shows that comorbid women appear to have higher risk for low ambulatory BP. ABPM could help physician in tailoring antihypertensive treatment, however, prospective studies are needed in order to precisely define clinical impact of low diastolic ambulatory BP, also considering the more appropriate timing of drug administration.[61]
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose.The authors thank Dr. Isabella Bagnaresi (Clinica Medica Unit, Azienda Ospedaliero-Universitaria S. Anna,Ferrara, Italy) for her important editorial assistance.
 Journal of Geriatric Cardiology2022年4期
Journal of Geriatric Cardiology2022年4期
- Journal of Geriatric Cardiology的其它文章
- Rotor hypothesis in the time chain of atrial fibrillation
- 3D vena contracta area in degenerative mitral regurgitation:cross-platform comparison in a single patient
- New-onset heart failure masking a massive retroperitoneal liposarcoma
- Invasive versus non-invasive hemodynamic monitoring of heart failure patients and their outcomes
- Implication of a novel truncating mutation in titin as a cause of autosomal dominant left ventricular noncompaction
- Trends and sex differences in atrial fibrillation hospitalization and catheter ablation at tertiary hospitals in China from 2013 to 2016
