Invasive versus non-invasive hemodynamic monitoring of heart failure patients and their outcomes
Fadi Kandah, Pooja Dhruva, Raj Shukla, Maedeh Ganji, Carlos Palacio, Emil Missov,Jose Ruiz-Morales
1. Internal Medicine, University of Florida College of Medicine-Jacksonville, Jacksonville, Florida, USA; 2. Division of Cardiology, University of Florida College of Medicine-Jacksonville, Jacksonville, Florida, USA
Acute decompensated heart failure (HF) is the most common cause of hospital admission in patients older than 65 years.Mean length of hospital stay is about 5-6 days and with a frequent number of hospital readmission rates of 25% to 50% at 30 days and 6-12 months, respectively.[1]Treatment options are vast and depend on certain patient characteristics, including hemodynamics, which drive the acute management. A popular modality to assess hemodynamics in acute HF is the right heart catheterization (RHC). While invasive, the use of RHC gives providers the opportunity to evaluate values that directly contribute to the management of the patient. These numbers can calculate the cardiac output as well as help establish the underlying etiology of the patient’s symptoms and guide therapy.[2]
Per Doshi, the use of right artery catheterization increased from 2010?2014 per 1000 hospitalizations compared to 2005?2010. The ESCAPE trial was a large trial that evaluated the use of RHC to guide therapy, however, results were shown to increase adverse events without affecting overall mortality and hospitalization.[3]It was not until its use was studied in patients with cardiogenic shock (CS) in which RHC was shown to be associated with lower mortality and in-hospital cardiac arrest.[4]Furthermore, another study compared RHC with N-terminal pro-B-type natriuretic peptide (NT-proBNP)measurements in the prognosis of chronic HF patients. It concluded that NT-proBNP was a better predictor of all-cause mortality with the benefit of being non-invasive.[5]The role of RHC is still not clearly defined and its necessity in guiding therapy of HF patients is controversial. It is also not wellknown which patient’s populations benefit most from it.
A retrospective study was conducted at a safetynet hospital in Jacksonville, Florida, USA. Through electronic medical record review, data was collected on HF admissions, procedures, medications,and medical history between January 2020 and December 2020. Inclusion criteria involved those patients over the age of 18 years who were admitted to the cardiac care unit. A total of 176 patients fitting this criteria were reviewed and stratified by age,gender, race, comorbidities, length of stay, ejection fraction (reducedvs.preserved), etiology of cardiomyopathy (ischemicvs.nonischemic), NT-proBNP and creatinine levels.
Statistical analysis was performed using SPSS 22.0 (SPSS Inc., IBM, Chicago, IL, USA). Categorical variables are presented as counts (percentages). Continuous variables are presented as mean ± SD or median (interquartile range) as appropriate. Differences were assessed using the Pearson’s chi-squared test and Mann-WhitneyUtest as appropriate. The study was approved by the regional Institutional Review Board. All authors were involved in data collection and interpretation of results.
This study resulted in 176 total patients. As shown in Table 1, out of these 176 patients, 95 patients were Caucasian and 81 patients were African American.139 patients had HF with reduced ejection fraction(HFrEF) and 37 patients had HF with preserved ejection fraction (HFpEF). Furthermore, 14 patients presented with ST-segment elevation myocardial infarction (STEMI). For our primary aim, this study showed that those who received RHC had a longer length of stay (11.5 days) than those who did not receive RHC (6.7 days). For our secondary aims, our results showed that there was a statistical difference in those who received RHC between ischemic cardiomyopathy and non-ischemic cardiomyopathy (41.8%vs.23.7%,P= 0.011). Caucasian patients were more likely to receive RHC than African American patients (40.0%vs.22.2%,P= 0.012). Patients presenting with STEMI received RHC more than those who did not receive RHC (71.4%vs.28.4%,P= 0.001). There was also a significant difference in those who received RHC that required inotropes during their hospital stay than those who did not receive RHC (61.4%vs.22.0%,P< 0.001). However,there was no statistical difference between the HFrEF group and HFpEF group (34.5%vs.21.6%,P= 0.134).
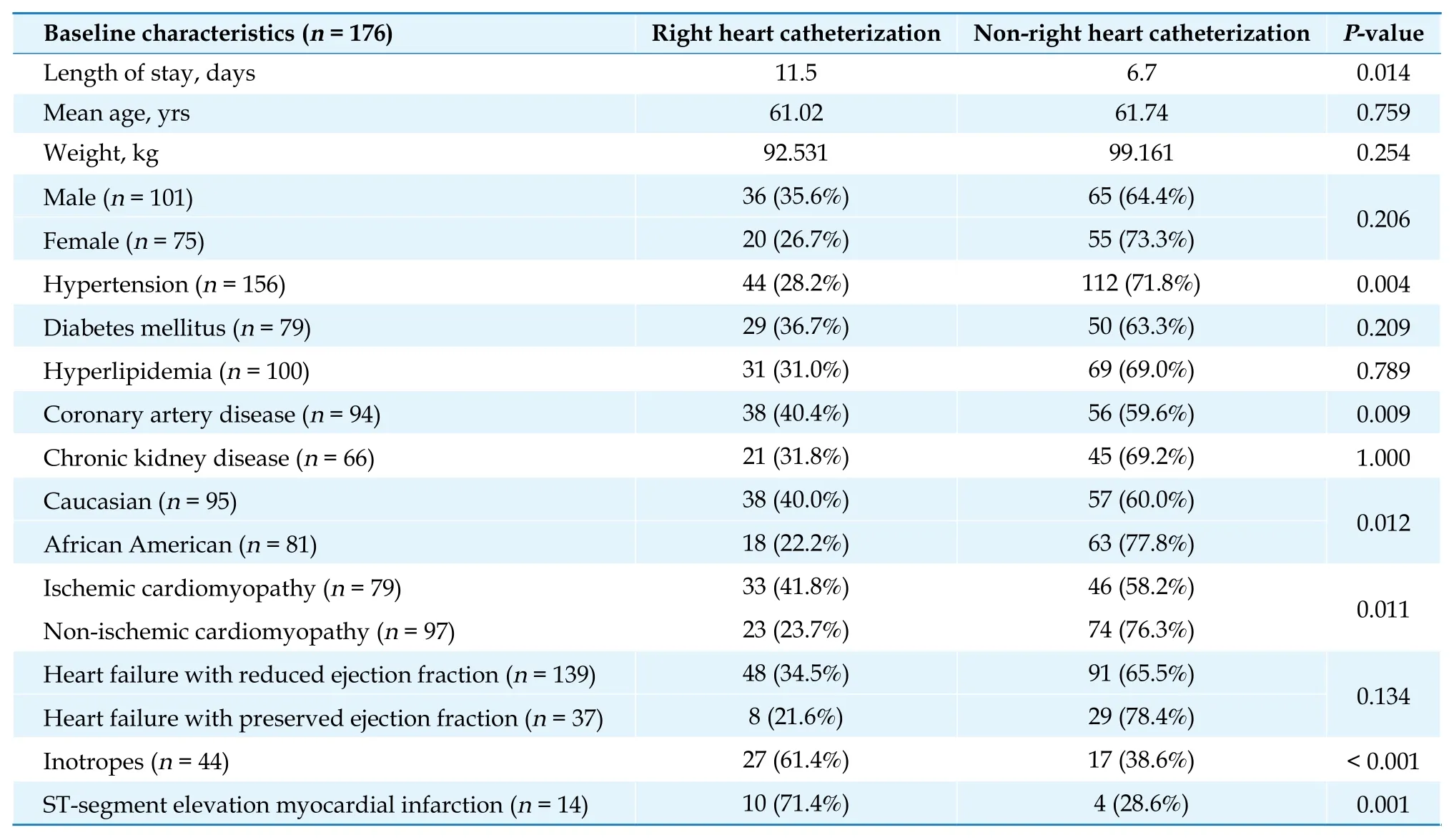
Table 1 Baseline characteristics between patients who received right heart catheterization versus those who did not receive right heart catheterization.
There was a greater difference in creatinine and NT-proBNP on admission and discharge in the RHC group, with creatinine showing statistical significance on both endpoints (P= 0.001, Table 2). There were no complications seen in any of the patients who underwent RHC.
While it was found that RHC was not associated with reduced hospital length of stay in patients presenting with acute decompensated HF, there was interesting data that was obtained about patient characteristics who received RHC. Certain patient populations have a significantly higher propensity to receive RHC without significant benefit in length of stay. This may be attributable to the fact that those who received RHC tended to be relatively sicker patients, with many of them either awaiting hospice and/or transfer to more advanced HF facilities. These same patients may have also been unresponsive to initial medical therapies prompting more invasive hemodynamic monitoring. One study shows that those who were not responsive to medical therapy had a change in therapy with improved mortality after having RHC performed.[5]This hesitance to place RHC at the beginning of hospitalization may be the cause of these patients to have a longer length of stay.
Interestingly, those patients who were more likely to receive RHC at the beginning of their hospitalization were those who presented with acute coronary syndrome. In our study, we focused on those who were admitted with STEMI. This patient population was more likely to receive RHC. However, in the GUSTO IIb and GUSTO III trials, those patients with STEMI that received RHC had increased 30-day mortality versus those who did not receive RHC.[6]Those that had the most benefit from RHC utilization were those in CS, as mentioned beforehand.[4,6]This is likely due to these patients having more dynamic day-to-day changes in values requiring changes in therapy.
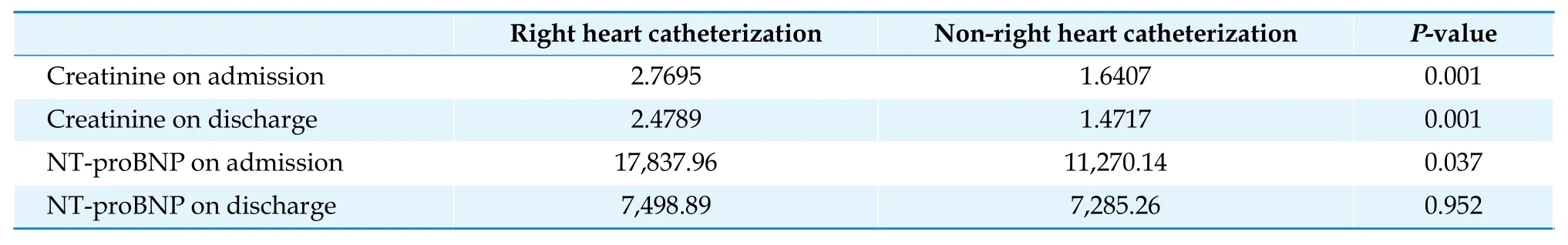
Table 2 Differences in creatinine and NT-proBNP on admission and discharge.
The RHC group was noted to have a significant decrease in NT-proBNP measurements compared to those that did not. A study compared RHC with NTproBNP measurements in the prognosis of chronic HF patients. It concluded that NT-proBNP was a better predictor of all-cause mortality with the benefit of being non-invasive.[7]This correlates well with the RHC group having significant decrease in NTproBNP levels. However, this study signifies that perhaps NT-proBNP levels alone can help guide therapy without the invasive hemodynamic monitoring and adverse effects that may be brought from it.It is important to note that there were no significant complications from any of the patients that received RHC in this study. The risk of major complications from RHC placement is less than 1% with a mortality rate of 0.05%.[8]This is operator dependent as well, meaning those institutions with less expertise may lean more on non-invasive methods for therapy.
Inherent bias may also play a role as those with these characteristics may be considered more difficult to manage. An interesting note is the discrepancy between races in those who received RHC. Caucasian patients tended to receive RHC more often than African American patients. African American patients tend to have a higher prevalence of comorbidities that lead to a higher rate of HF hospital admissions.These patients are often overlooked and their etiology may be more complex than expected.[9]Socioeconomic factors may also play a significant role as increased length of hospitalization and more invasive procedures may provide a financial burden for the patient and hospital.
The utility of the RHC in certain patient populations continues to be an evolving domain of interest. There are still no definitive guidelines for its use and evidence is still lacking for its role in therapy. However,there still tends to be a propensity to use hemodynamic monitoring in those patients who present with more instability, whether it is CS, acute coronary syndrome or requiring inotropes. With this, study do not shows improvements in outcomes in these populations.Further investigation is warranted to determine a guideline directed approach to manage RHC in certain hospitalized patients.
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose.
 Journal of Geriatric Cardiology2022年4期
Journal of Geriatric Cardiology2022年4期
- Journal of Geriatric Cardiology的其它文章
- Rotor hypothesis in the time chain of atrial fibrillation
- 3D vena contracta area in degenerative mitral regurgitation:cross-platform comparison in a single patient
- New-onset heart failure masking a massive retroperitoneal liposarcoma
- Implication of a novel truncating mutation in titin as a cause of autosomal dominant left ventricular noncompaction
- Trends and sex differences in atrial fibrillation hospitalization and catheter ablation at tertiary hospitals in China from 2013 to 2016
- Tongmai Yangxin Pill combined with metoprolol or metoprolol alone for the treatment of symptomatic premature ventricular complex: a multicenter, randomized, parallel-controlled clinical study
