Paracentral acute middle maculopathy after diagnostic cerebral angiography in a patient with a contralateral carotid-cavernous fistula
Lidia Remol Sargues, Javier Montero Hernndez, Clara Monferrer Adsuara, Nuria Gonzlez Girn,Alicia Gracia Garca, Vernica Castro Navarro, Enrique Cervera Taulet
Department of Ophthalmology, Consorcio Hospital General Universitario of Valencia, Av. Tres Cruces 2, Valencia 46014,Spain
Dear Editor,
I am Dr. Lidia Remolí Sargues from Consorcio Hospital General Universitario of Valencia. We write to present a case of paracentral acute middle maculopathy (PAMM) in a patient with a contralateral carotid-cavernous fistula (CCF)after cerebral diagnostic angiography.
CCFs are anomalous communications between the carvenous sinus and carotid arterial system that can cause severe ocular and neurological morbidity. CCFs have a wide spectrum of clinical presentations depending on the anatomy and flow of the lesion[1-3]. The most common ocular findings are exophthalmos, epibulbar loops, motility disturbances, and glaucoma[4]. The vast majority of patients show only ipsilateral signs[2].
PAMM is a recently described clinical finding related to a selective ischemia in the intermediate and deep retinal capillary plexus. It is characterized by a hyperreflective band-like lesion in the inner nuclear layer (INL) in the optical coherence tomography (OCT). PAMM is more frequent in males between 50 and 60 years old and can be asymptomatic. PAMM has an ischemic microvascular origin and has been associated with numerous ocular disorders, systemic diseases, medications,and medical procedures[5-7].
Case Report
A 69-year-old male presented with redness and vision loss of his left eye (OS). His medical history was significant for the presence of arterial hypertension and type 2 diabetes, and for the history of a vertebrobasilar stroke 3 years ago. He had an ophthalmological history of a primary open angle glaucoma treated with latanoprost once daily. Best-corrected visual acuity (BCVA) was 80 letters (20/25) in the right eye (OD) and 75 letters (20/32) in the OS. Pupillary response, extraocular motility, and intraocular pressures were normal. Anterior segment examination revealed dilated and corkscrew scleral and episcleral vessels in the OS and a significative nuclear cataract that justified the visual acuity of the OS. Posterior segment examination was normal.
A diagnosis of CCF was suspected, so neuroimaging was performed. Brain magnetic resonance (MR) angiography objectified a dilation of the left cavernous sinus and the left superior ophthalmic vein, and no masses or structural abnormalities were seen. Cerebral angiography confirmed the presence of a dural CCF, with a shunt among left ascending pharyngeal artery (a branch of the external carotid artery) and left vertebral artery (a branch of the subclavian artery) with the left cavernous sinus. Therefore, a diagnosis of dural CCF was confirmed and endovascular embolization of the dural CCF was scheduled by the interventional neuroradiology service.
One month later, the patient presented to the emergency room with a vision loss of his OS. BCVA was 80 letters(20/25) in the OD and 20 letters (20/400) in the OS. Pupillary response, extraocular motility, and intraocular pressures were unremarkable. Anterior segment examination showed a progression of the nuclear cataract of the OS that explained the vision loss. Posterior segment examination illustrated a yellow-gray lesion following a band pattern along the superior cilioretinal artery in the OD (Figure 1). OCT revealed hyperreflectivity between the inner plexiform layer (IPL) and the outer plexiform layer (OPL) in the macular region of the OD (Figure 2). Infrared imaging objectified a well-defined hyporreflective lesion along the superior cilioretinal artery in the OD (Figure 2). En face OCT demonstrated hyperreflectivity in an arteriolar distribution in the deep retina, and OCT angiography revealed a juxtapapillary area of capillary dropout in both superficial and deep capillary plexus and in the choriocapillaris (Figure 2). The juxtapapillary area of capillary dropout in the choriocapillaris was probably due to signal attenuation secondary to hyper-reflectivity between IPL and ONL. Fluorescein angiography (FA) and indocyanine green angiography (ICGA) confirmed the presence of a hypofluorescent and hypocianescent lesion in an arteriolar pattern (Figure 1).
A diagnosis of PAMM secondary to a cilioretinal artery obstruction was confirmed. Because of that, laboratory evaluation (including complete blood count, erythrocyte sedimentation rate, coagulation tests, renal function, and electrolytes) was performed to rule out secondary causes.Furthermore, the patient denied a previous and recent viral illness. A diagnosis of PAMM secondary to diagnostic cerebral angiography was suspected.
DISCUSSION
PAMM is the clinical finding of an ischemic injury in the intermediate and deep retinal capillary plexus that can be associated with multiple ocular disorders, systemic diseases or medications, such as diabetic retinopathy, retinal artery occlusion, retinal vein occlusion, orbital compression injury,CCF, migraine, antiphospholipid syndrome, postviral or postvaccination syndrome, amphetamines, caffeine, and oral contraceptives. Furthermore, PAMM has been associated with coronary procedures, aortic procedures, aortography,and carotid interventions. It can be difficult to demonstrate an association between PAMM and a single underlying cause, because it can be caused by several factors. The clinical symptoms are variable, ranging from no symptoms to paracentral scotoma or vision loss. In asymptomatic patients, such as our case, OCT may be an essential diagnostic procedure that allows an early detection. Currently, there is no treatment for PAMM, although its management should be targeted toward the identification and treatment of related vascular risk factors, when present, in order to avoid visual and neurological sequelae[3,5-8].
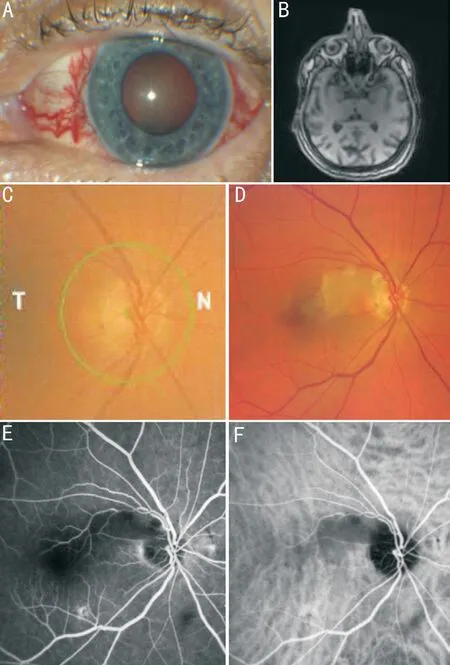
Figure 1 Anterior segment examination of the left eye (OS), brain magnetic resonance imaging (MRI), and fundus examination of the right eye (OD) A: Anterior segment examination showed prominent, dilated, and corkscrew scleral and episcleral vessels in the OS; B: Brain MRI revealed a slight dilation of the left cavernous sinus; C: Fundus imaging at baseline was unremarkable, except for peripapillary atrophy; D: Fundus imaging after cerebral angiography showed a grayer lesion following a band pattern along the superior cilioretinal artery in the OD. E, F: Fluorescein angiography and indocyanine green angiography confirmed the presence of a hyperfluorescent and hypercianescent lesion in an arteriolar pattern corresponding with the band-like lesion visualized in the fundus imaging.
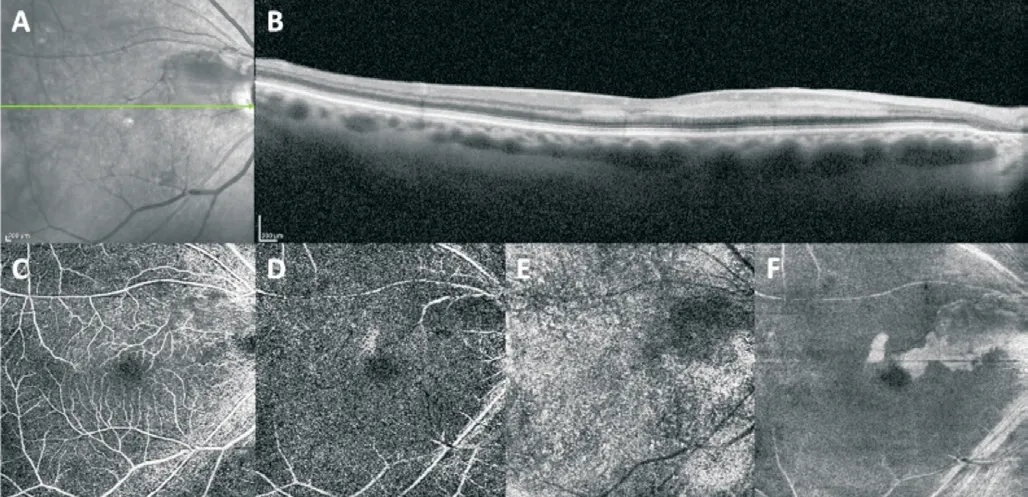
Figure 2 Optical coherence tomography (OCT) and optical coherence tomography angiography (OCTA) of the right eye (OD)A: Infrared imaging showed a well-defined hyporreflective lesion in an arteriolar pattern in the OD; B: OCT illustrated hyper-reflectivity between the inner plexiform layer and the outer plexiform layer in the macular region of the OD; C-E: OCTA confirmed a juxtapapillary area of capillary dropout in both superficial and deep capillary plexus and in the choriocapillaris; F: En face OCT demonstrated hyperreflectivity in an arteriolar distribution in the deep retina.
The cavernous sinus is a complex venous structure that is anastomosed anteriorly and posteriorly between the right and left sides. CCFs are anomalous communications between the carvenous sinus and carotid arterial system. Specifically, dural CCFs result from shunts between the cavernous sinus and small dural branches of the internal or external carotid artery.Dural CCFs are usually formed by multiple connections and may be induced by microtraumas or vessel wall disorders[1-2,4].Because of that, clinical presentation of dural CCFs is variable,including contralateral and even bilateral involvement. Those that drain posteriorly can be asymptomatic, and present with isolated cranial nerve palsies, or even drain to cerebral vessels,causing intracranial haemorrhage. Also, posterior drainage sometimes becomes anterior, with orbital congestion[1,4].Bilateral signs can be seen in the 9% of the cases and retinal ischemia affects the 11% of the patients, according to de Keizer’s[4]report. Nevertheless, this association has to be taken into account as well, as it is shown in this report.
The contralateral ischemic damage due to CCF in our case could be associated with elevated venous pressure in the orbital compartment. The orbital venous congestion may compromise retinal perfusion, leading to retinal arterial occlusion[3]. This association is rare, but medical comorbidities of our patient (arterial hypertension, type 2 diabetes, and a history of a vertebrobasilar stroke), could produce a previous retinal vascular alteration, favoring the ischemia of the intermediate and deep capillary plexus. Furthermore,PAMM has been reported in association with endovascular procedures, but otherwise has not been described after a diagnostic cerebral angiography[3,7-8]. In these cases, iatrogenic rupture of atheromatous plaques and endothelial injury during microcatheter insertion might be the origin of PAMM[7-8].Diagnostic cerebral angiography is an invasive procedure that involves carotid and vertebral artery catheterisation. The risk of complications is higher in patients with cardiovascular disease, as in our patient. Atherosclerotic plaque disruption and vessel dissection during catheterisation, and heparininduced thrombocytopenia could cause thromboembolism phenomena[9]. The diagnosis of PAMM after the diagnostic cerebral angiography in the context of the cardiovascular morbidity of our patient (arterial hypertension, type 2 diabetes,vertebrobasilar stroke history, and dural CCF) suggests that diagnostic cerebral angiography could be the trigger factor,albeit the establishment of a causal association was not possible.
In conclusion, PAMM should be considered a clinical finding that reflects an ischemic damage secondary to an underlying ocular or systemic vasculopathy. Therefore, it is crucial that ophthalmologists investigate the origin causes in order to uncover vascular risk factors that could be life-threatening. In addition, the absence of symptoms in some cases of PAMM could underestimate the prevalence of this entity after a diagnostic cerebral angiography. Thus, OCT becomes an essential tool in its detection.
ACKNOWLEDGEMENTS
Conflicts of Interest:Remolí Sargues L,None;Montero Hernández J,None;Monferrer Adsuara C,None;González Girón N,None;Gracia García A,None;Castro Navarro V,None;Cervera Taulet E,None.
 International Journal of Ophthalmology2022年11期
International Journal of Ophthalmology2022年11期
- International Journal of Ophthalmology的其它文章
- Optical coherent tomography angiography observation of macular subinternal limiting membrane hemorrhage in CO poisoning: a case report
- Choroidal folds associated with carotid cavernous fistula:a case report
- Role of the ultra-wide-field imaging system in the diagnosis of pigmented paravenous chorioretinal atrophy
- A rare combination of late-onset post-LASlK keratectasia after early-onset central toxic keratopathy
- Gastrointestinal microbiome and primary Sj?gren’s syndrome: a review of the literature and conclusions
- lnsights on the possibility of SARS-CoV-2 transmission through the eyes
