Pre-hospital delay in patients with acute myocardial infarction in China: findings from the Improving Care for Cardiovascular Disease in China-Acute Coronary Syndrome (CCC-ACS) project
Dan-Qing HU, Yong-Chen HAO, Jun LIU, Na YANG, Yi-Qian YANG, Zhao-Qing SUN,Dong ZHAO, Jing LIU, On behalf of the CCC-ACS investigators
Department of Epidemiology, Beijing Anzhen Hospital, Capital Medical University, Beijing Institute of Heart, Lung and Blood Vessel Diseases, Beijing, China
ABSTRACT OBJECTIVE To describe the duration of the pre-hospital delay time and identify factors associated with prolonged pre-hospital delay in patients with acute myocardial infarction (AMI) in China. METHODS Data were collected from November 2014 to December 2019 as part of the Improving Care for Cardiovascular Disease in China-Acute Coronary Syndrome (CCC-ACS) project. A total of 33,386 patients with AMI admitted to the index hospitals were included in this study. Two-level logistic regression was conducted to explore the factors associated with the pre-hospital delay and the associations between different pre-hospital delay and in-hospital outcomes. RESULTS Of the 33,386 patients with AMI, 70.7% of patients arrived at hospital ≥ 2 h after symptom onset. Old age, female, rural medical insurance, symptom onset at early dawn, and non-use of an ambulance predicted a prolonged pre-hospital delay (all P < 0.05). Hypertension and heart failure at admission were only significant in predicting a longer delay in patients with ST-segment elevation myocardial infarction (STEMI) (all P < 0.05). A pre-hospital delay of ≥ 2 h was associated with an increased risk of mortality [odds ratio (OR) = 1.36, 95% CI: 1.09-1.69, P = 0.006]and major adverse cardiovascular events (OR = 1.22, 95% CI: 1.02-1.47, P = 0.033) in patients with STEMI compared with a pre-hospital delay of < 2 h. CONCLUSIONS Prolonged pre-hospital delay is associated with adverse in-hospital outcomes in patients with STEMI in China.Our study identifies that patient characteristics, symptom onset time, and type of transportation are associated with pre-hospital delay time, and provides focuses for quality improvement.
Early invasive strategies are the key to improving the survival of patients with acute myocardial infarction (AMI).[1,2]Previous attention focused on door-to-balloon (DTB) time has resulted in significant improvements; however, several studies have confirmed that mortality is strongly correlated with the total ischemic time and less so with the DTB interval.[3-5]As the longest component of ischemic time, the pre-hospital delay from symptom onset to admission is an important point of focus.[6]A previous study showed that the benefit of a short DTB time was restricted to patients who presented early.[7]These results suggest that although it is imperative to minimize the DTB time as an inseparable part of the ischemic time, the importance of shortening the pre-hospital delay should not be ignored.
Several studies reported the duration of the pre-hospital delay and examined the factors associated with the prolonged pre-hospital delay. These studies showed notable differences in the lengths of pre-hospital delay among different countries.[8-10]According to data from the Global Registry of Acute Coronary Events study,the pre-hospital delay of patients with ST-segment elevation myocardial infarction (STEMI) was shortest in Australia/New Zealand (median: 2.2 h) and longest in Argentina and Brazil (median: 4.0 h).[10]In China, the China PEACE (China Patients-Centered Evaluative Assessment of Cardiac Events) study reported an average time to hospital of 4.0 h for AMI,and certain factors, such as rural medical insurance,failure to recognize symptoms as cardiac, and a low household income, were associated with a longer prehospital delay.[11]However, the latest national study about the scenario of pre-hospital delay in China was conducted from 2012 to 2014.[11]An up-to-date evaluation of pre-hospital delay in patients with AMI in China is warranted. In addition, the pathological process of patients with non-ST-segment elevation myocardial infarction (NSTEMI) is different as compared with STEMI, but few studies have explored the clinical outcomes of the prolonged pre-hospital delay in NSTEMI patients.[12]
Using nationwide data from the Improving Care for Cardiovascular Disease in China-Acute Coronary Syndrome (CCC-ACS) project, we herein provide an up-to-date estimation of the pre-hospital delay time;explore the factors associated with the pre-hospital delay; and investigate the association between the prehospital delay and in-hospital outcomes among patients with STEMI and patients with NSTEMI in China.
METHODS
Study Design and Population
The CCC-ACS project is a nationwide quality improvement registry program that focuses on improving the quality of care for patients with acute coronary syndrome (ACS). As a collaborative initiative of the American Heart Association and the Chinese Society of Cardiology, 150 tertiary hospitals participated from 2014 to 2015, and 82 secondary hospitals and 9 tertiary hospitals further participated from 2017 to 2018.Every month, the first 20-30 patients with ACS and 10-20 patients with ACS were recruited consecutively from tertiary hospitals and secondary hospitals,respectively. Detailed information about the design and methodology of the program have been published previously.[13]From November 2014 to December 2019, 94,623 patients with AMI were registered based on the principal discharge diagnosis. Only directly admitted patients within 24 h of symptom onset were included in this study. The flowchart of participant inclusion and exclusion is shown in Figure 1. The project is registered at ClinicalTrials.gov (NCT02306616) and was approved by the Institutional Review Board of Beijing Anzhen Hospital, Capital Medical University,Beijing, China (No.2014018), with a waiver for informed consent.
Data Collection
Clinical data were obtained from patients’ medical records. To ensure the accuracy of the reported data,around 5% of reported cases were randomly selected for validation of the original medical records by third-party research associates, and the medical record abstraction achieved an accuracy of over 95%.
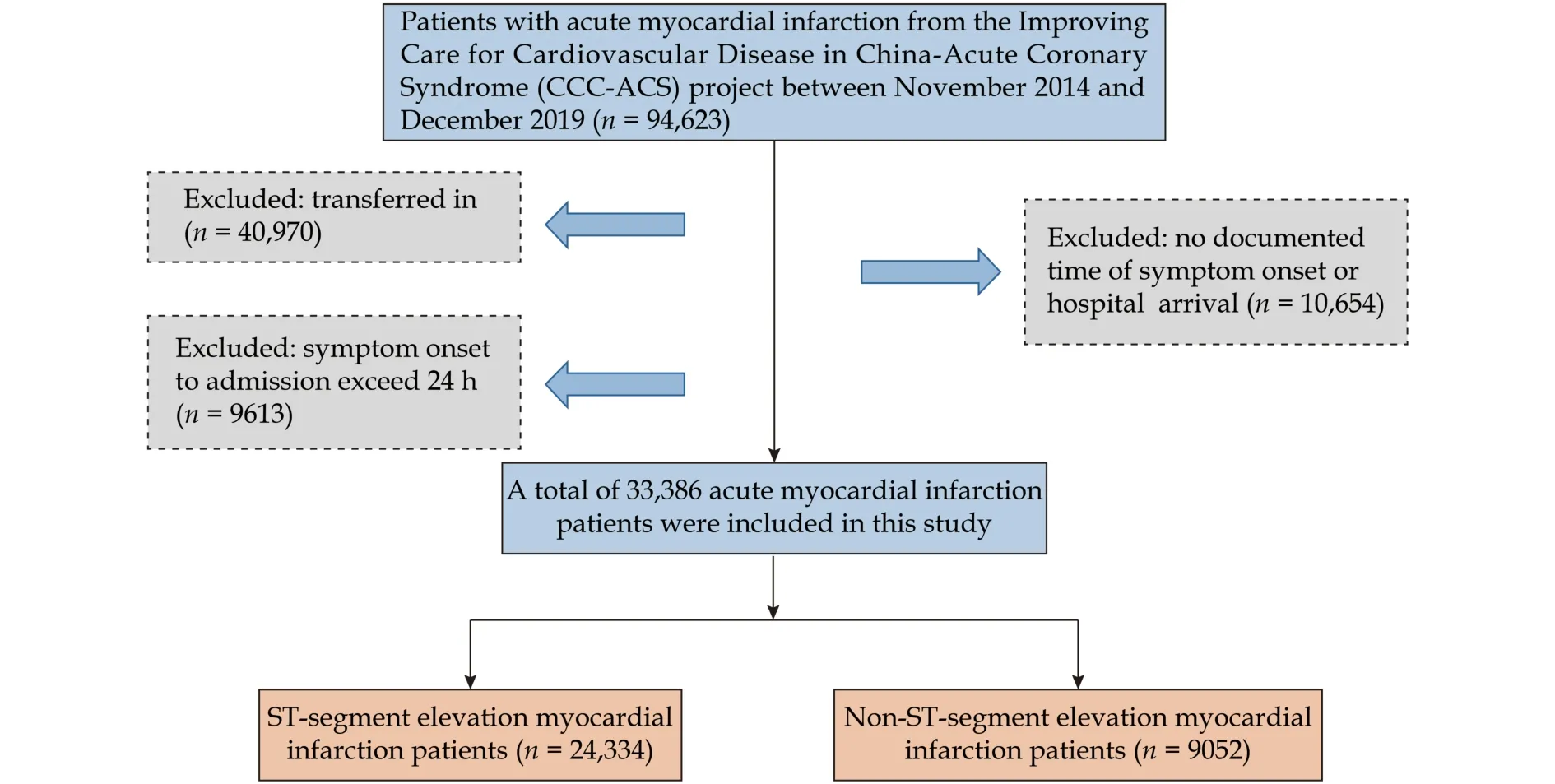
Figure 1 Flowchart of the screening process for the selection of eligible participants.
Study Variables
Patient characteristics included demographics (age,sex, marriage, and medical insurance), risk factors (hypertension, diabetes mellitus, elevated low-density lipoprotein cholesterol, smoking, and renal insufficiency),disease history [heart failure (HF), atrial fibrillation,stroke/transient ischemic attack, and coronary heart disease (CHD)], symptom onset time (onset at early dawn and onset at working time), severe clinical conditions at admission (HF, cardiogenic shock, and cardiac arrest), and transportation by ambulance. Hospital characteristics included hospital grade, regional economic level, and geographic area. Early revascularization therapies included fibrinolysis and primary percutaneous coronary intervention for STEMI and timely percutaneous coronary intervention for NSTEMI. At the same time, we also summarize the definitions of these variables (supplemental material, Table 1S).
The duration of pre-hospital delay was defined as the time from symptom onset to hospital arrival, which was retrieved by reviewing patients’ medical records.A delay of ≥ 2 h was defined as a prolonged pre-hospital delay, to keep consistency with previous studies.[10,11]
In-hospital outcomes included major adverse cardiovascular events (MACEs) during hospitalization and mortality. MACEs were defined as a combination of cardiac death, re-infarction, and stroke.
Statistical Analysis
Variables are described as mean ± SD or median(interquartile range) for continuous variables or counts(percentages) for categorical variables, and were compared with the independent Student’st-test, the Mann-WhitneyUtest, or the Pearson’s chi-squared test. Twolevel logistic regression models (patient-level and hospital-level) were used to account for clustering of patients within hospitals to determine the predictors of prolonged pre-hospital delay and explore the in-hospital outcomes of patients with AMI with different prehospital delays. The potential factors influencing the prolonged pre-hospital delay in the two-level model were selected based on the univariable analysis (P<0.05). The confounding factors adjusted in the multivariable analysis of the association between pre-hospital delay and in-hospital outcomes included all patient characteristics listed in Table 1, as well as early revascularization therapies. The proportion of patients with missing data and the strategies used to manage missing data are described and summarized in detail (supplemental material, Table 2S). R software(version 3.6.2, http://www.R-project.org) and Stata software (version 14.0; Stata, College Station, TX, USA)were used for data analysis. Two-sidedP-value < 0.05 were considered statistically significant.
RESULTS
A total of 33,386 patients with AMI from 241 hospitals in China with pre-hospital delay information,including 24,334 STEMI patients and 9052 NSTEMI patients, were enrolled in the overall sample (Figure 1).
Distribution of Pre-hospital Delay
The median pre-hospital delay of patients with AMI was 3.3 (1.6-7.0) h. The median pre-hospital delay of NSTEMI patients was longer than that of STEMI patients [4.2 (2.0-9.5) hvs.3.0 (1.5-6.0) h]. Overall, 70.7%of patients with AMI arrived at hospital ≥ 2 h after symptom onset (69.1% for STEMI and 75.0% for NSTEMI), and 30.2% of patients with AMI presented for medical care more than 6 h after symptom onset (26.6%for STEMI and 40.1% for NSTEMI) (Figure 2).
Patient and Hospital Characteristics by Duration of Pre-hospital Delay
The characteristics across different pre-hospital delay groups are summarized in Table 1. Patients with a longer pre-hospital delay were older and more likely to be female, while those with a shorter pre-hospital delay were more likely transported by ambulance;however, an ambulance was used in less than 20% of cases in both groups (Table 1). Hospital characteristics,such as a higher hospital grade, were associated with a longer time from symptom onset to admission, and the median delay was longest in regions with a less developed economy and in Northwest China (Table 1 and supplemental material, Table 3S).
Factors Associated with Pre-hospital Delay
In patients with STEMI, age ≥ 65 years [odds ratio (OR) = 1.26, 95% CI: 1.19-1.35,P< 0.001], female (OR =1.22, 95% CI: 1.13-1.32,P< 0.001), rural medical insurance compared to urban medical insurance (OR = 1.49,95% CI: 1.36-1.63,P< 0.001), hypertension (OR = 1.09,95% CI: 1.02-1.16,P= 0.006), symptom onset at early dawn (OR = 1.58, 95% CI: 1.47-1.71,P< 0.001), and HF at admission (OR = 1.22, 95% CI: 1.06-1.41,P=0.005) were independent predictors of a prolonged pre-hospital delay (≥ 2 h) after multivariable adjustment. Previous CHD (OR = 0.82, 95% CI: 0.74-0.90,P< 0.001), cardiogenic shock at admission (OR = 0.80,95% CI: 0.68-0.94,P= 0.006), cardiac arrest at admission (OR = 0.63, 95% CI: 0.51-0.77,P< 0.001), and transportation by ambulance (OR = 0.61, 95% CI: 0.56-0.66,P< 0.001) were significantly associated with early presentation (Figure 3).

Table 1 Characteristics of patients with ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction with different pre-hospital delay.
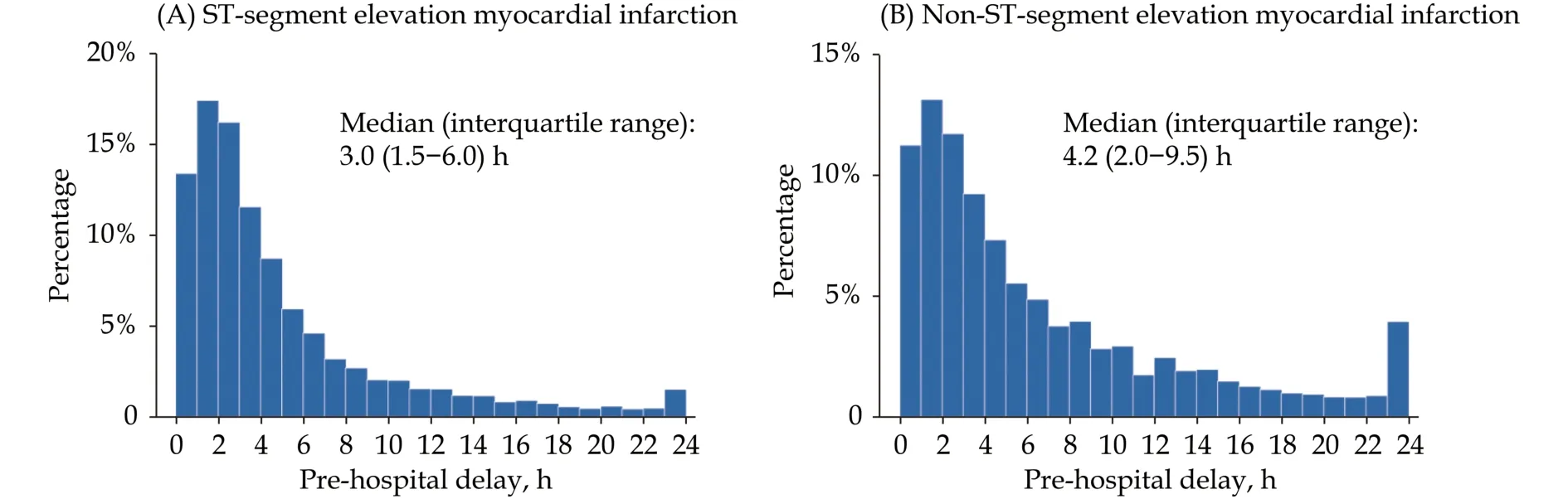
Figure 2 Distribution of pre-hospital delay time in patients hospitalized with ST-segment elevation myocardial infarction (A) and non-ST-segment elevation myocardial infarction (B).
Similar factors were associated with a pre-hospital delay of ≥ 2 h in patients with NSTEMI. For example,old age, female, rural medical insurance, and symptom onset at early dawn were independent factors associated with a prolonged pre-hospital delay (allP<0.05), whereas transportation by ambulance was a significant predictor of a shorter pre-hospital delay (OR =0.48, 95% CI: 0.40-0.57,P< 0.001) (Figure 3).
Association Between Pre-hospital Delay and Inhospital Outcomes
For patients with STEMI, a prolonged pre-hospital delay (≥ 2 h) was associated with an increased risk of in-hospital mortality (OR = 1.36, 95% CI: 1.09-1.69,P=0.006) and MACEs (OR = 1.22, 95% CI: 1.02-1.47,P=0.033). For patients with NSTEMI, no significant association was observed between pre-hospital delay (≥ 2 h)and in-hospital outcomes, even in patients with a very high risk based on risk stratification (supplemental material, Table 4S).
DISCUSSION
In this up-to-date nationwide real-world registry,over 70% of patients with AMI suffered a prolonged pre-hospital delay of ≥ 2 h. Old age, female, rural medical insurance, hypertension, symptom onset at early dawn, and non-use of an ambulance were associated with a prolonged pre-hospital delay. Prolonged pre-hospital delay was associated with an increased risk of in-hospital outcomes for patients with STEMI.
Although a great improvement in pre-hospital delay was observed compared with the China PEACE study from 2012 to 2014 (3.3 hvs.4.0 h), the median delay (3.0 h for STEMI and 4.2 h for NSTEMI) in our study was still higher than previous reports in Western countries (1.7-2.3 h for STEMI and 1.9-2.7 h for NSTEMI)and Asian countries, such as South Korea (145 min for STEMI and 196 min for NSTEMI).[10,11,14]These findings suggest room for improvement in the prehospital delay for patients with AMI in China.
Understanding the risk factors for pre-hospital delay is the cornerstone to improving the situation. A previous study identified that patients with a lack of awareness about STEMI are likely to prolong their time to treatment.[15]Many patients initially fail to recognize myocardial infarction symptoms and misattribute their symptoms to other causes, which may lead to a longer decision delay. For example, older patients, female patients, and patients complicated with hypertension are more likely to present with atypical symptoms of AMI.[16-18]In addition, chronic angina in patients with STEMI with HF also makes it difficult to distinguish myocardial infarction from chronic chest pain.[19]For patients with rural insurance, the lower level of health literacy among rural residents compared with their urban counterparts might, in part, explain the longer delay.[20]In addition, the higher proportion of patients with out-of-pocket costs was also a potential reason for the delayed presentation.[21]In our analysis, previous CHD emerged as an independent predictor of early presentation after symptom onset. We supposed that these patients had more knowledge about AMI, which encouraged them to seek medical care early after the onset of suspected symptoms.
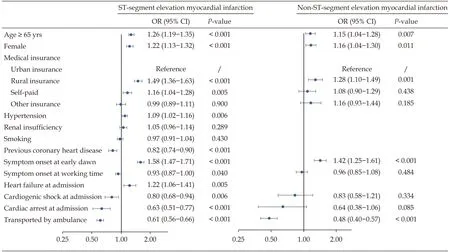
Figure 3 Factors associated with pre-hospital delay in the two-level logistic regression model.
The onset time also affected the pre-hospital delay.Specifically, patients with symptom onset at early dawn tended to wait longer before accessing medical care in our study. It was previously reported that patients may not like to bother others unless the symptoms are extremely severe during periods when most people are asleep.[22]However, impaired consciousness and hypotension in severe clinical conditions, such as cardiogenic shock or cardiac arrest, may prompt them to attend hospital.
Our results extend previous findings by indicating that transportation by ambulance is associated with a shorter pre-hospital delay.[23]
Unfortunately, more than 80% of patients in this analysis avoided calling for an emergency ambulance,which is greater than the 40% reported in the United States in 2011.[23]This might be one of the important causes of the prolonged pre-hospital delay of patients with AMI in China.
We also observed large gaps in presentation time among different hospital grades and economic levels.Compared with patients at tertiary hospitals, those at secondary hospitals were less likely to arrival at hospital late. A similar result was observed in the China Acute Myocardial Infarction registry, which showed that patients at lower-level hospitals were less likely to suffer a longer pre-hospital delay than those at higher-level hospitals.[24]We also found that in areas of lower economic status, the duration of pre-hospital delay was relatively longer. The low density of high-level hospitals (secondary and tertiary) in low economic areas may be partly responsible for their poor accessibility.[25]Moreover, the pre-hospital delay also varied among different geographic regions, and the long prehospital delay in Northwest China was in accordance with the lowest economic level of this area.[26]
In this study, we also investigated the prognosis of patients with AMI with different pre-hospital delay.For patients with STEMI, similar to several prior studies, we found that a late presentation (≥ 2 h) was independently correlated with adverse in-hospital clinical outcomes in patients with STEMI.[8,27]For patients with NSTEMI, few studies have reported the effects of pre-hospital delay on mortality. Although the Korea Acute Myocardial Infarction Registry-National Institutes of Health found that a pre-hospital delay of≥ 24 h was associated with an increased risk of threeyear all-cause mortality in patients with NSTEMI, no significant differences in in-hospital all-cause mortality were observed,[28]which is consistent with the relationship between the pre-hospital delay and in-hospital outcomes in our study.
The findings of this study suggest the urgency of shortening pre-hospital delays. Continuous efforts to raise public awareness of the symptoms suggestive of AMI are important, especially in older patients, female patients, and patients complicated with hypertension who are vulnerable to longer pre-hospital delays.The use of an ambulance is encouraged to achieve early diagnosis and therapy. Furthermore, medical resources also affect the pre-hospital delay. The discrepancy in the delay among hospital and economic levels may be related to the imbalanced distribution of medical resources, which demonstrates the importance of increasing medical resource allocation and elevating hospital reperfusion treatment to provide all patients with equal access to health services.
STRENGTHS AND LIMITATIONS
To the best of our knowledge, this is the most recent nationwide study of pre-hospital delay in patients with AMI in China. The data of our study provide useful evidence for future research on reducing the delay in medical care in patients with STEMI and patients with NSTEMI. However, the present study had several limitations. Firstly, survival bias might exist as patients who died of AMI outside of hospital were not included in our study. Secondly, the time of symptom onset was obtained by patient self-reporting and may thus not be accurate. This study only included patients who were directly admitted to hospital within 24 h of symptom onset; thus, the estimated effect of recall bias is limited.
CONCLUSIONS
In this nationwide registry, a substantial proportion of patients with AMI in China demonstrated a prolonged delay in seeking medical care. Strategies to shorten patients’ decision times, to encourage the use ambulances, and to provide reliable medical resources are warranted.
ACKNOWLEDGMENTS
This study was supported by the CCC-ACS Project(NCT02306616), which is a collaborative project of the American Heart Association and the Chinese Society of Cardiology. The American Heart Association received funding from Pfizer through an independent grant for learning and change and AstraZeneca as a quality improvement initiative. All authors had no conflicts of interest to disclose. The authors thank all participating hospitals for their data contribution to the CCC-ACS Project. Please see our summary of the names of principal investigators and participating centers(supplemental material, Table 5S).
 Journal of Geriatric Cardiology2022年4期
Journal of Geriatric Cardiology2022年4期
- Journal of Geriatric Cardiology的其它文章
- Ambulatory diastolic blood pressure: a marker of comorbidity in elderly fit hypertensive individuals?
- Essen score in the prediction of cerebrovascular events compared with cardiovascular events after ischaemic stroke or transient ischaemic attack: a nationwide registry analysis
- Tongmai Yangxin Pill combined with metoprolol or metoprolol alone for the treatment of symptomatic premature ventricular complex: a multicenter, randomized, parallel-controlled clinical study
- Trends and sex differences in atrial fibrillation hospitalization and catheter ablation at tertiary hospitals in China from 2013 to 2016
- Implication of a novel truncating mutation in titin as a cause of autosomal dominant left ventricular noncompaction
- Invasive versus non-invasive hemodynamic monitoring of heart failure patients and their outcomes
